Indocyanine Green-Guided Precision in a Left Lateral Sectionectomy for Hepatocellular Carcinoma
Article information
Abstract
Parenchyma-sparing anatomical resection is recommended in patients with hepatocellular carcinoma due to the presence of underlying liver disease. More precise hepatectomy has been enabled by recent technical advancements, including negative staining with indocyanine green following ligation of the corresponding Glissonean pedicle, which offers intraoperative guidance by delineating the resection plane in real-time. Herein, we present a case of laparoscopic left lateral sectionectomy that used this staining technique.
Introduction
Liver resection remains the cornerstone of the curative interventions used for hepatocellular carcinoma (HCC). However, a significant proportion of HCC cases present with underlying liver dysfunction, necessitating careful preoperative assessment of future remnant liver volume and function, as well as overall patient condition [1]. In such instances, a parenchymal-sparing anatomical resection is recommended. This approach includes precise techniques such as selective Glissonean pedicle ligation and corresponding parenchymal dissection. Recent advancements in surgical technology have introduced the use of real-time indocyanine green (ICG)-based fluorescence imaging for hepatectomy [2]. In this procedure, resection margins are determined post-ligation of the Glissonean pedicle via venous ICG injection. ICG fluorescence imaging thereby enables a precise delineation of the intersegmental plane during surgery [3]. We here present a case of a hepatic resection performed using this technique.
Case Presentation
A 54-year-old male patient diagnosed with HCC during a follow-up for hepatitis B virus-induced liver cirrhosis underwent two transarterial chemoembolization procedures and radiofrequency ablation (RFA). He was transferred to our hospital due to a marginal recurrence after RFA. Subsequent preoperative imaging revealed a tumor in segment II (Fig. 1A). The patient’s alpha-fetoprotein level was 2.5 ng/mL, and he was classified as Child-Pugh A with an Eastern Cooperative Oncology Group performance status of 0.
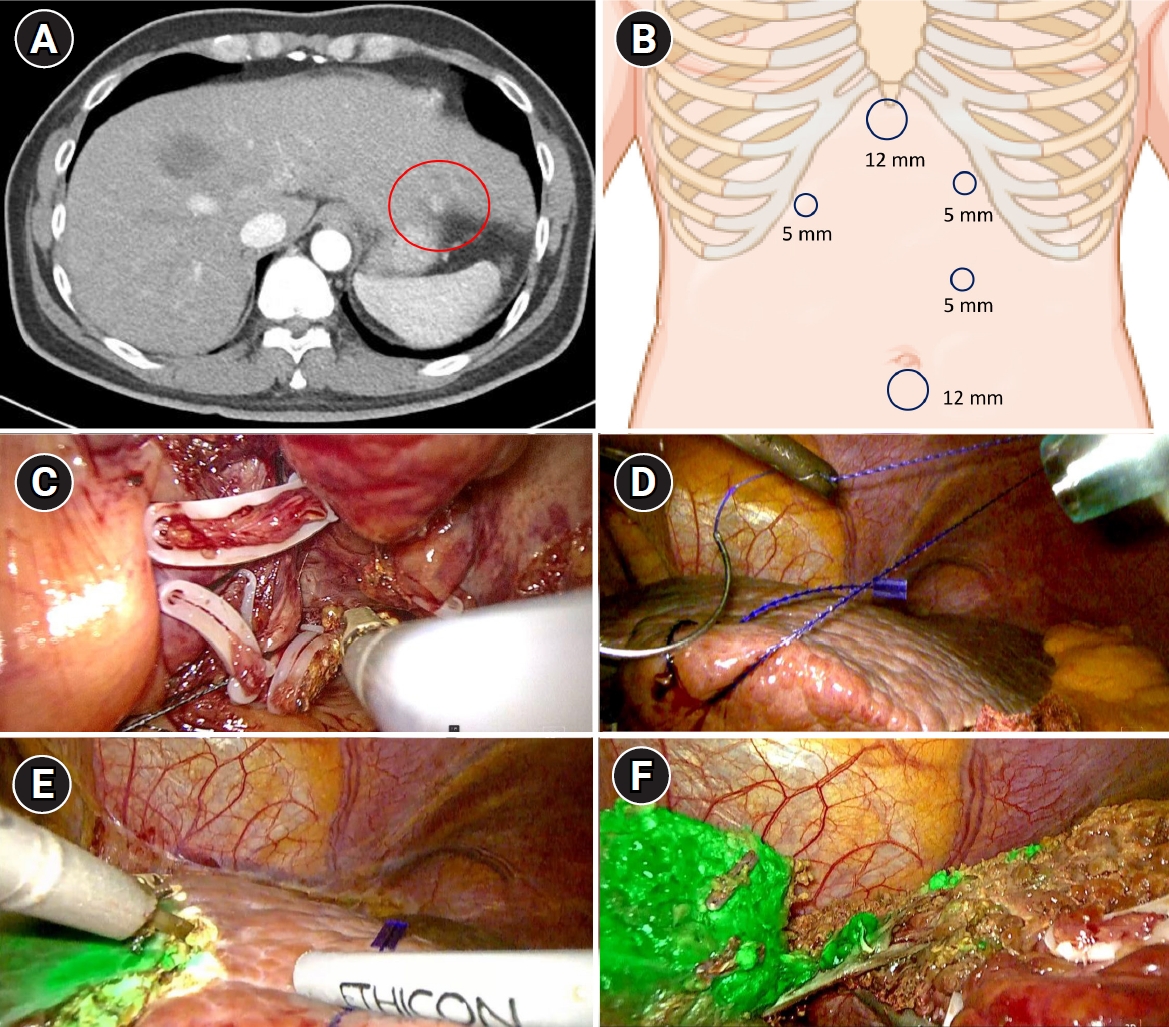
(A) A liver nodule with marginal recurrence in segment II following radiofrequency ablation (red circle). (B) Port placement for laparoscopic left lateral sectionectomy. (C) The Glissonean pedicles for segments II and III were ligated and transected. (D) The left liver was retracted to the left using a barbed suture. (E) The resection plane was marked along the demarcation line after the administration of indocyanine green. (F) The left hepatic vein was exposed after parenchymal dissection along the fluorescent plane.
Surgery was performed in which the patient was placed in the supine position and, under general anesthesia, a 12 mm umbilical port was inserted for a laparoscopic camera. The pneumoperitoneum was established at 12–14 mmHg. Four additional ports were placed as follows: a 12 mm epigastric port for the Cavitron ultrasonic surgical aspirator, a 5 mm right subcostal port for the surgeon’s left hand, a 5 mm left subcostal port for the assistant, and a periumbilical port for the external Pringle maneuver (Fig. 1B).
A plastic tape was placed around the hepatoduodenal ligament, with the ends pulled out through a tube and secured with a Kelly clamp to prepare for the Pringle maneuver. The falciform ligament was dissected, the common trunk of the left and middle hepatic veins was identified, and the left coronary ligament was dissected. The left liver was elevated, and the Glissonean pedicles for segments II and III were isolated, and transected (Fig. 1C). The demarcation line was checked, and 2.5 mg of ICG was administered intravenously for real-time fluorescence imaging to delineate the resection margin. Prior to parenchymal dissection, the round ligament was ligated using an endoloop and retracted to the right side. The left liver was sutured with barbed thread, and the peritoneum was sutured and fixed (Fig. 1D) [4]. This suturing further secured the resection field as the procedure progressed (as depicted in the video).
Liver resection was performed using an advanced bipolar system for the left hand and a Cavitron ultrasonic surgical aspirator after application of the Pringle maneuver (Fig. 1E). Parenchymal dissection was carried out along the border between the non-fluorescent and fluorescent areas. The left hepatic vein was transected using an endoscopic stapler (Fig. 1F). The total surgical time was 1 hour and 21 minutes, with an estimated blood loss of 10 mL. The patient was discharged without complications at 7 days postoperatively and was under close monitoring for tumor recurrence at the time of writing. The patient has been under follow-up for 22 months without evidence of recurrence. This study was approved by the Institutional Review Board (IRB) of the Asan Medical Center (IRB No: 2024-1178). Informed consent from the patient was waived due to anonymized data.
Discussion
Anatomical resection is considered the optimal surgical approach for HCC, particularly for ensuring the complete removal of tumors within the corresponding portal vein territory [1]. Notably, however, its reproducibility has been challenged in the past by difficulties in consistently identifying reliable intrahepatic landmarks while preserving the resection plane [5]. The advent of ICG-guided parenchymal transection has introduced a highly reproducible and more precise method for liver resection [6]. Following inflow control, ICG fluorescence delineates the liver tissue designated for resection, thereby improving surgical accuracy.
Meta-analyses of ICG-guided liver resections have since demonstrated significant benefits, including reduced blood transfusion rates, shorter postoperative hospital stays, and improved R0 resection rates, without an increase in postoperative complications [7]. Despite these advantages, however, proper inflow control is essential with this protocol, as incomplete control may lead to inaccurate staining of the resection margin, potentially compromising surgical outcomes. In cases requiring intervention at the third-order branch Glisson’s pedicles for subsegmentectomy, a parenchymal-first approach prior to ICG injection is recommended [8].
This technique thus ensures more precise delineation of the resection margin and facilitates a safer, more effective liver resection. The presented case further underscores the feasibility of utilizing ICG fluorescence imaging in hepatic resections, demonstrating that this method allows for real-time, precise identification of resection margins, potentially enhancing surgical outcomes.
Notes
Disclosure
No potential conflict of interest relevant to this article was reported.
Author contributions
Conceptualization: WL, KPH, ML, MS; Data curation: YP, KBS, JHL, DWH, SCK; Formal analysis: WL, KPH; Investigation: KPH, DWH; Methodology: MS, KBS, JHL; Supervision: KBS, JHL, DWH, SCK; Writing–original draft: WL, KPH, ML, MS, YP; Writing–review & editing: KPH, MS, YP, KBS, JHL, DWH, SCK.

