Laparoscopic Extended Totally Extraperitoneal Hernia Repair with Posterior Component Separation with Transversus Abdominis Release for a Recurrent Incisional Hernia
Article information
Abstract
A patient with multiple comorbidities, including hypertension, type 2 diabetes, hyperlipidemia, and edema, and a prior history of abdominal surgery presented to the gastrointestinal department with a recurrent incisional hernia larger than 10 cm. The patient underwent laparoscopic extended totally extraperitoneal (e-TEP) hernia repair under general anesthesia. The bilateral retrorectal spaces were accessed via three trocars, followed by midline crossover in the upper abdomen and caudal dissection along the fascial defect. Due to the large size of the defect and the anticipated tension, posterior component separation (PCS) with transversus abdominis release (TAR) was performed, with careful preservation of the neurovascular bundles running anterior to the head of the transversus abdominis muscle. After separate closure of the posterior and anterior layers using barbed sutures, a mesh was placed in the intercomponent space to avoid direct contact with intraperitoneal structures. Closed-suction drains were placed bilaterally to prevent seroma formation. The procedure was completed successfully, and the patient experienced no complications. The patient was discharged without complications. A follow-up computed tomography scan demonstrated the integrity of the hernia repair, with progressive resolution of fat infiltration and fluid collection. Laparoscopic e-TEP hernia repair with PCS and TAR provides a safe and effective approach for managing complex recurrent incisional hernias. This technique enables tension-free closure with mesh placement while minimizing intra-abdominal complications.
Introduction
Incisional hernia is one of complications following abdominal surgeries, including open and minimally invasive surgery. This case report presents a patient in the sixth decade of life, with a complex surgical and medical history, who underwent laparoscopic extended totally extraperitoneal (e-TEP) hernia repair with posterior component separation (PCS) with transversus abdominis release (TAR) for a large recurrent incisional hernia.
PCS, derived from the principles of the Rives–Stoppa repair, involves dissection of the retrorectal space from the posterior rectus sheath toward the semilunar line, creating a broad and well-vascularized plane suitable for mesh placement. The transversus abdominis (TA) and internal oblique muscles (IO) serve as key structural components that contribute to abdominal wall integrity. Mobilizing the TA from the overlying IO allows for expansion of the abdominal cavity while preserving the function of the IO. Additional TAR, incising the head of the TA, allowing dissection to the preperitoneal plane and facilitating extensive medialization of the abdominal wall. It is important to be cautious to avoid injury to the neurovascular bundles, which run just anterior to the head of the TA and perforate into the rectus muscle, as these are essential for maintaining rectus muscle function [1].
Case Presentation
The patient had a history of distal pancreatectomy followed by open incisional hernia repair without mesh several years ago. The patient had multiple comorbidities, including hypertension (managed with antihypertensive agents), type 2 diabetes mellitus (treated with oral hypoglycemics and insulin), hyperlipidemia (treated with lipid-lowering medication), and peripheral edema (managed with diuretics).
Considering the patient’s complex medical and surgical history, along with a large recurrent hernia defect measuring approximately 10 cm, a laparoscopic e-TEP hernia repair was planned.
Surgical procedure
In the supine position, the surgical site was prepared and draped for laparoscopic surgery under general anesthesia. The patient was positioned with hyperextension of the lower back and hip joint, using the hernia site as a reference point, in order to optimize access of laparoscopic instruments and facilitate optimal access to the hernia defect. A 12-mm trocar was inserted in the left upper quadrant of the abdominal wall to access the left retrorectal space and enable dissection of the preperitoneal area. CO2 was insufflated into the retrorectal space to create working space, after which an additional 5 mm trocar was inserted into the left abdomen through the expanded retrorectal area. Additionally, a 12-mm trocar was inserted in the right upper quadrant, providing access to the right retrorectal space for further dissection (Fig. 1).
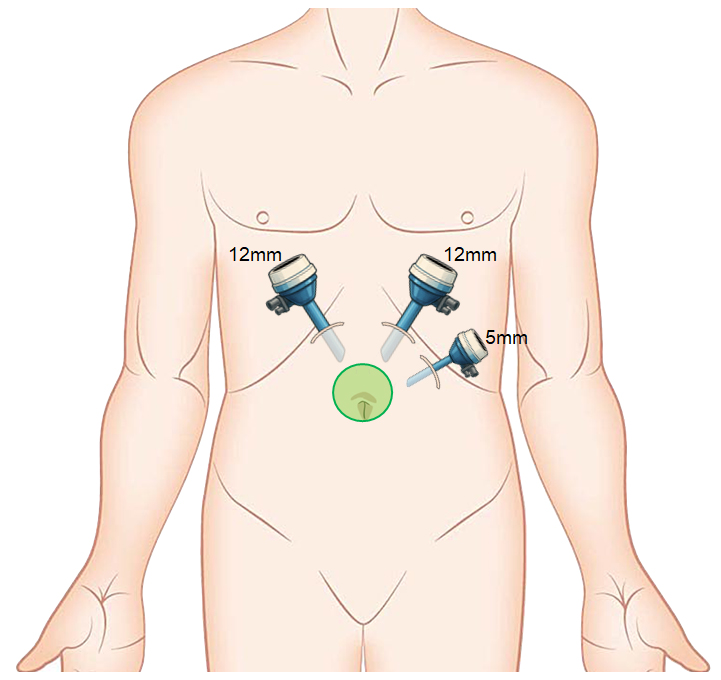
Trocar placement on the abdominal wall. A 12-mm trocar was inserted in the left upper quadrant to access the left retrorectal space. A 5-mm trocar was placed in the left abdomen, and another 12-mm trocar was inserted in the right upper quadrant for access to the right retrorectal space. The green circle indicates the location of the incisional hernia sac.
Midline crossing was performed to access the contralateral retrorectal space without entering the intraperitoneal cavity. During this step, a yellow fat pad representing the falciform ligament was visualized and served as an anatomical guide. This step is essential in the extended TEP approach, as it connects the bilateral retrorectal spaces, allowing for a wider working space and appropriate mesh placement. Extensive postoperative adhesions were noted and required meticulous adhesiolysis. A large incisional hernia was identified, approximately 10 cm in size, and the hernia sac was carefully dissected along its margin at the fascial defect (Fig. 2). Owing to the large size of the hernia defect, even a minimal PCS from posterior rectus sheath laterally toward the linea semilunaris permitted direct visualization of the head of the TA. TAR, involving careful division of the head of the TA, was performed to achieve adequate tension-free closure of the posterior layer (Fig. 3). The posterior component was closed with a barbed suture. The anterior component was also closed with a barbed suture, incorporating plication of the redundant hernia sac beneath the skin flap to minimize dead space and reduce the risk of seroma formation (Fig. 4). A mesh with two anchoring threads was placed in the intercomponent space, between the anterior and posterior component, and transfascial fixation was performed. Closed-suction drains were placed bilaterally within the intercomponent space to prevent seroma formation. A detailed surgical procedure is illustrated in video.
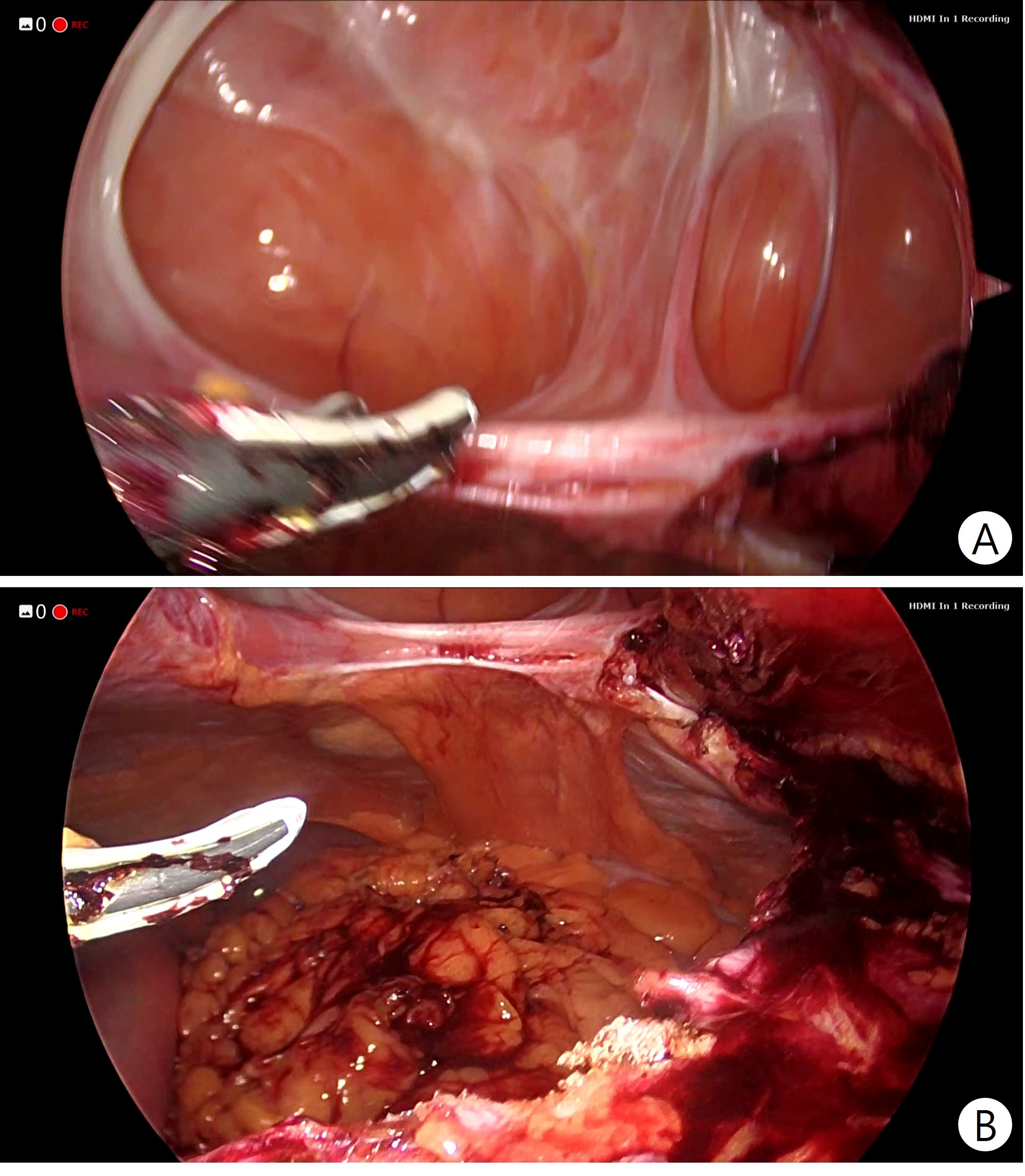
Intraoperative findings of recurrent incisional hernia. (A) A large recurrent incisional hernia was identified following adhesiolysis. (B) The posterior component was dissected from the margin of the hernia sac.
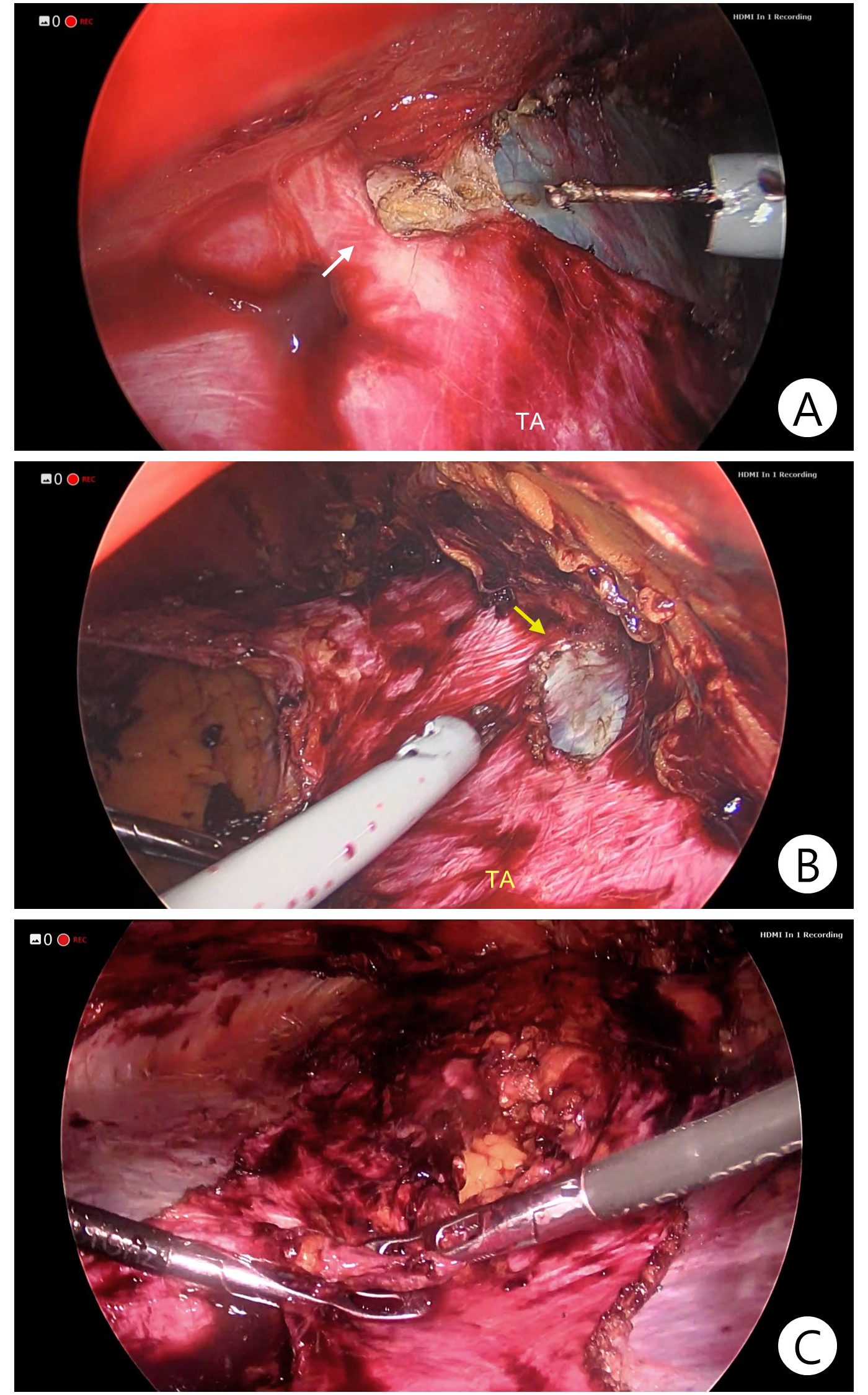
Posterior component separation with transversus abdominis release (TAR). (A) Division of the head of the transversus abdominis muscle (TA) on the left side (white arrow). (B) Division of the head of the TA on the right side (yellow arrow). (C) Tension-free approximation of the bilateral posterior components after TAR.
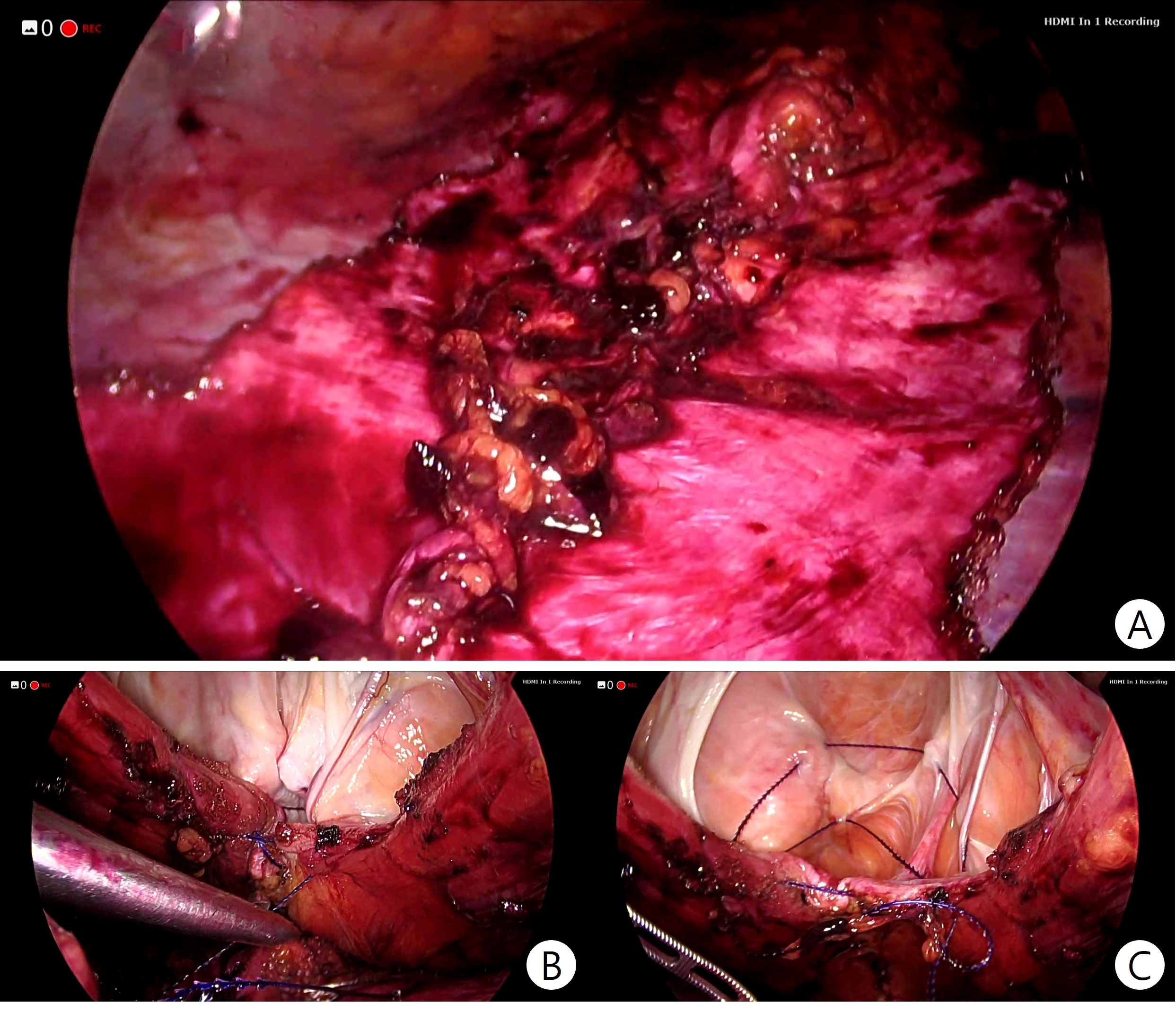
Closure of the posterior and anterior components. (A) The posterior component was closed with a barbed suture. (B, C) The anterior component was closed with a barbed suture, incorporating plication of the redundant hernia sac to minimize dead space and reduce the risk of seroma formation.
Postoperative course
The postoperative course was uneventful, followed by discharge after a short hospital stay. Initial follow-up computed tomography (CT) confirmed the integrity of the hernia repair, with mild fat infiltration and a small fluid collection between the anterior compartment and the hernia sac. No symptoms or signs of infection were observed. Subsequent follow-up CT demonstrated decreased fat infiltration and fluid collection, with no abnormal findings on physical examination.
Discussion
This case highlights the challenges of managing recurrent incisional hernia in patients with complex medical and surgical histories. Laparoscopic e-TEP hernia repair offers several advantages: 1) In cases of recurrent hernias, which are often associated with extensive adhesions that increase the risk of iatrogenic bowel injury [2], accessing the space between the anterior and posterior components rather than directly entering the intraperitoneal space reduces the risk of direct bowel injury even when adhesiolysis is required; 2) when the defect is large and fascial approximation would result in excessive tension, simultaneous PCS with TAR can be performed immediately to achieve a tension-free closure [1]; 3) by closing the anterior and posterior components separately and placing the mesh within the intercomponent space, direct contact between the mesh and intraperitoneal structures is avoided, thereby minimizing the risk of adhesion formation [3]; 4) e-TEP repair is also associated with less postoperative pain, faster recovery, and lower recurrence rate compared to open hernia repair [4,5].
Given these benefits, laparoscopic e-TEP hernia repair with PCS with TAR serves as a promising approach for managing recurrent incisional hernias, even in patients with complex surgical and medical histories. Careful patient selection, precise surgical technique, and consistent postoperative monitoring with imaging are essential to optimize surgical outcomes. Nevertheless, this report describes a single case without long-term follow-up or comparative data, which limits the generalizability of the findings. Further studies involving larger patient cohorts and extended follow-up are warranted to validate the broader applicability of this technique.
Notes
Disclosure
No potential conflict of interest relevant to this article was reported.
Author contributions
Conceptualization: SHK (Kong); Data curation: SHK (Kim); Formal analysis: SHK (Kim); Investigation: SHK (Kim); Methodology: SHK (Kim); Writing–original draft: SHK (Kim); Writing–review & editing: KP, CK, JK, DJP, HJL, SHK (Kong)

