Abstract
- Arteriovenous fistula (AVF) creation is crucial for patients with end-stage renal disease requiring long-term hemodialysis, due to its superior long-term patency and lower complication rates compared to arteriovenous grafts. This paper presents detailed techniques and a step-by-step tutorial for AVF creation—including radiocephalic, brachiocephalic, and brachiobasilic fistulas—offering valuable insights for both novice and experienced surgeons.
-
Keywords: Arteriovenous fistula, Renal dialysis, Vascular surgical procedures, Surgical procedures, operative, Education, medical
Introduction
Arteriovenous fistula (AVF) creation is the gold standard for hemodialysis access in patients with end-stage renal disease (ESRD) due to its superior long-term patency and lower complication rates compared to arteriovenous grafts [1]. A good surgical technique is essential to obtain optimal results and reduce the risk of primary failure [2].
A supplementary video (Video 1) is included to illustrate the step-by-step approach to a radiocephalic AVF, providing practical guidance for both novice and experienced surgeons.
Case Presentation
A 60-year-old male patient with ESRD was referred for vascular access creation. The patient had underlying hypertension and diabetes mellitus but no prior history of vascular surgeries or central venous catheter placements. Preoperative duplex ultrasound mapping revealed suitable vessels for AVF creation at the left wrist and upper arm.
This study was approved by the Institutional Review Board (IRB) of Eulji University Uijeongbu Hospital, Korea (IRB No. UEMC 2024-12-010) and written informed consent was obtained from the patient.
Preoperative assessment
• Vessel mapping: Duplex ultrasound was used to assess the diameter and quality of the radial artery and cephalic vein. A radial artery diameter ≥2 mm and a cephalic vein diameter ≥2.5 mm were considered suitable for AVF creation.
• Patient evaluation: Comprehensive medical history and physical examination were conducted to identify comorbid conditions that might affect surgery or fistula maturation.
Surgical procedures
The surgical approach to AVF creation varies depending on patient-specific anatomy and surgeon preference. Key considerations include the size and quality of the vessels, the choice of suture material, and the type of skin incision. The following outlines commonly used techniques for AVF creation, acknowledging that variations exist and should be tailored to individual patient needs.
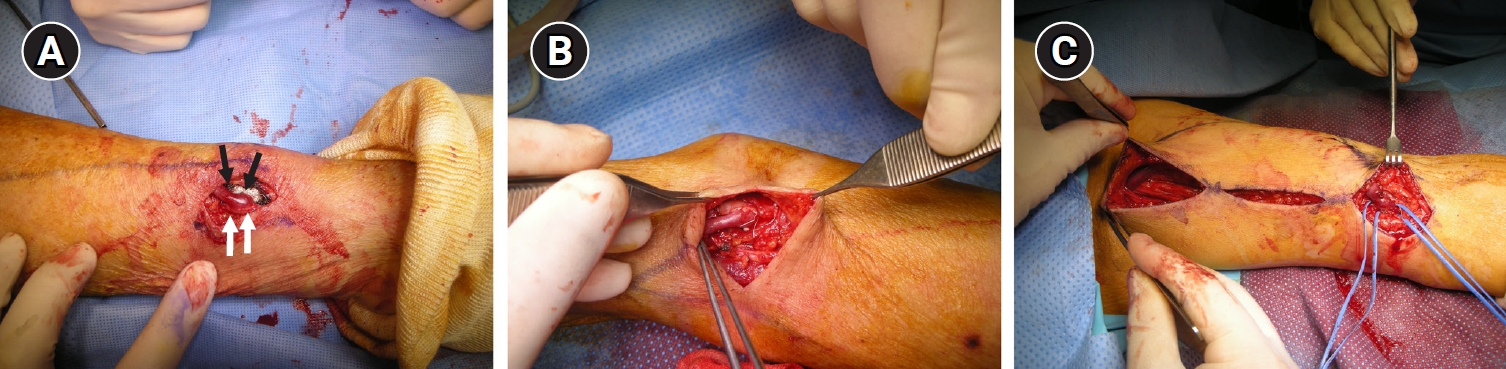
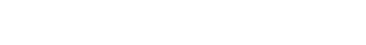
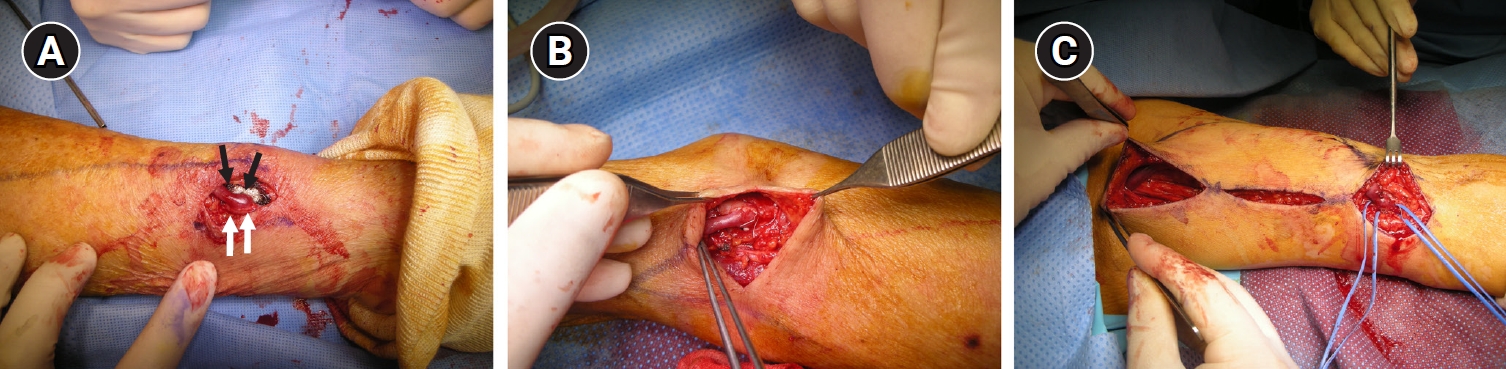
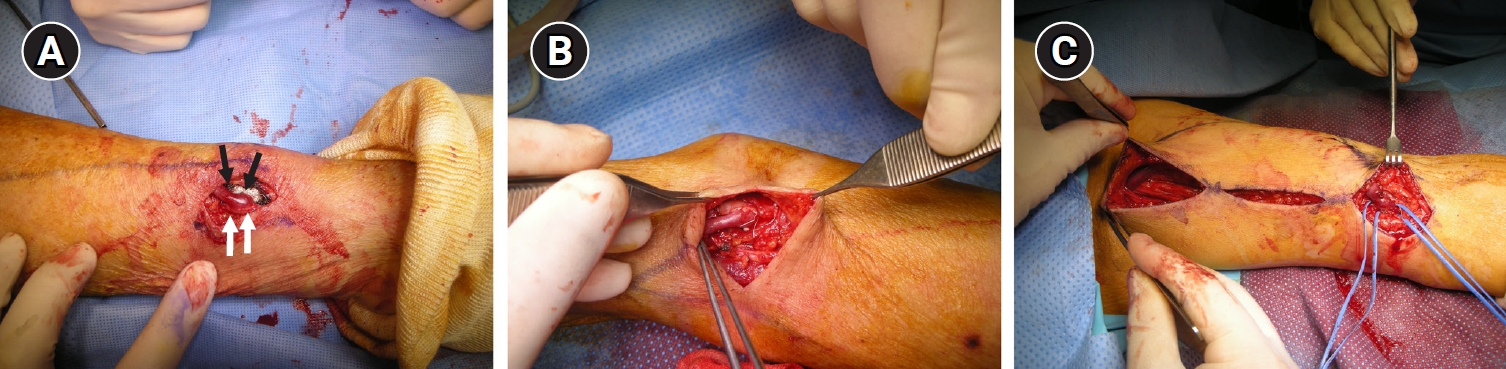
Radiocephalic arteriovenous fistula at the wrist
The patient was positioned supine with the left arm extended on an arm board under local anesthesia with sedation. A 5 cm longitudinal incision was made over the radial artery and cephalic vein at the wrist (Fig. 1A). The cephalic vein was identified and carefully dissected proximally to allow for a tension-free anastomosis, while the radial artery was exposed with care to preserve surrounding nerves and structures. Both vessels were mobilized adequately to prevent tension at the anastomosis site, and venous branches were ligated to increase the vein’s mobility. After irrigating the vessels with heparinized saline and trimming the vessel ends to healthy tissue, an end-to-side anastomosis was performed using continuous 7-0 polypropylene sutures under loupe magnification. The choice of suture material for the anastomosis can vary; commonly used sutures include 6-0 or 7-0 polypropylene or other monofilament sutures. In this procedure, continuous 7-0 polypropylene sutures were used under loupe magnification for an end-to-side anastomosis. Key technical considerations included gentle handling of the vessels to prevent spasm, precise suture placement to ensure lumen patency, and minimizing manipulation to reduce the risk of intimal hyperplasia. Upon completion, clamps were released, and a palpable thrill and audible bruit confirmed the success of the anastomosis. Hemostasis was achieved with careful inspection of the anastomosis site, and the incision was closed in layers using absorbable sutures for subcutaneous tissue and non-absorbable sutures for the skin.
Brachiocephalic arteriovenous fistula
In cases where distal vessels are inadequate, a brachiocephalic AVF can be created. A transverse incision was made over the antecubital fossa (Fig. 1B), and the cephalic vein and brachial artery were exposed and mobilized. The cephalic vein was dissected proximally, and the brachial artery was carefully isolated. An end-to-side anastomosis was performed, and the choice of suture material may include 5-0 or 6-0 polypropylene or other suitable sutures. In this case, 6-0 polypropylene sutures were used. The cephalic vein was spatulated to match the diameter of the brachial artery, ensuring optimal hemodynamics and reducing turbulence at the anastomosis site. After completing the anastomosis, flow was established, and hemostasis was confirmed before closing the incision appropriately.
Brachiobasilic arteriovenous fistula with transposition
For patients lacking suitable superficial veins, a brachiobasilic AVF with vein transposition is an effective alternative. A two-stage procedure was performed (Fig. 1C). In the first stage, a longitudinal incision along the medial aspect of the upper arm was made to mobilize the basilic vein, which was then prepared for an end-to-side anastomosis with the brachial artery using 6-0 polypropylene sutures, though suture size may vary between 5-0 and 7-0 based on surgeon preference and vessel size. After allowing time for maturation, the second stage involved transposing the matured basilic vein superficially through a subcutaneous tunnel to facilitate easy cannulation. Care was taken to prevent kinking or torsion of the vein during transposition, which could compromise flow. Alternative techniques include performing the transposition in a single stage or utilizing different incision approaches, such as creating a superficialized straight-line basilic vein transposition. The choice between one-stage and two-stage procedures depends on factors such as vein size, patient comorbidities, and surgeon experience. Successful flow and hemostasis were confirmed, and the incision was closed in layers.
Postoperative care
Patients were monitored for immediate postoperative complications such as bleeding, thrombosis, or infection. Physical examinations and duplex ultrasounds were conducted regularly to assess fistula maturation. Successful maturation was defined by adequate flow rates and vein diameter suitable for dialysis needle cannulation. The patients began hemodialysis using the new AVF within 4 to 6 weeks postoperatively without any significant complications.
Discussion
Selecting the appropriate type of AVF and surgical technique is crucial and depends on patient-specific factors such as vessel size, quality, and previous access sites [3]. The radiocephalic AVF is preferred due to its distal location, preserving proximal sites for future access. However, when distal vessels are unsuitable, proximal options like brachiocephalic or brachiobasilic AVFs are considered.
Technical considerations
• Vessel handling: Gentle manipulation reduces the risk of vasospasm and intimal injury.
• Anastomosis technique: Precise suture placement ensures patency and reduces turbulence.
• Tension-free connection: Adequate mobilization prevents anastomotic stress and promotes maturation.
• Use of magnification: Enhances visualization and accuracy during the procedure.
Training and education
Competency in AVF creation is essential for vascular surgery trainees. A structured, step-by-step tutorial ensures systematic skill acquisition, emphasizing patient safety and surgical proficiency. Progression through training phases with mentor approval guarantees preparedness at each stage.
Conclusion
Arteriovenous fistula creation is a fundamental procedure in vascular surgery, essential for providing reliable hemodialysis access to patients with ESRD. Mastery of various surgical techniques and individualized patient care are paramount to optimizing outcomes and extending the lifespan of vascular access sites. The standardized methods and training protocols presented can serve as a guideline for trainees and practicing surgeons alike.
Disclosure
No potential conflict of interest relevant to this article was reported.
Author contributions
Data curation, Formal analysis: JIK; Investigation: CSS; Methodology: CSS, JIK; Project administration: CSS; Resources: JIK; Supervision: CSS; Validation: JIK; Visualization: JIK; Writing–original draft, Writing–review & editing: CSS, JIK.
Fig. 1.(A) Intraoperative view of a radiocephalic arteriovenous fistula at the wrist. The radial artery (white arrows) and cephalic vein (black arrows) are carefully dissected for tension-free anastomosis. (B) Brachiocephalic arteriovenous fistula in the antecubital fossa. The cephalic vein is mobilized and anastomosed end-to-side to the brachial artery. (C) Brachiobasilic arteriovenous fistula with transposition. The basilic vein is first anastomosed to the brachial artery and subsequently transposed superficially.
REFERENCES
- 1. Vascular Access 2006 Work Group. Clinical practice guidelines for vascular access. Am J Kidney Dis. 2006;48 Suppl 1:S176-S247.ArticlePubMed
- 2. Rooijens PP, Tordoir JH, Stijnen T, Burgmans JP, Smet de AA, Yo TI. Radiocephalic wrist arteriovenous fistula for hemodialysis: meta-analysis indicates a high primary failure rate. Eur J Vasc Endovasc Surg. 2004;28:583-589.ArticlePubMed
- 3. Sidawy AN, Spergel LM, Besarab A, Allon M, Jennings WC, Padberg FT Jr, et al. The Society for Vascular Surgery: clinical practice guidelines for the surgical placement and maintenance of arteriovenous hemodialysis access. J Vasc Surg. 2008;48:2S-25S.
Citations
Citations to this article as recorded by

 , Ji Il Kim
, Ji Il Kim

 PubReader
PubReader ePub Link
ePub Link Cite this Article
Cite this Article
 KSSSG
KSSSG