Abstract
- Robotic transabdominal preperitoneal (R-TAPP) inguinal hernia repair offers enhanced visualization, ergonomic comfort, and improved instrument control compared to conventional laparoscopy. Although laparoscopic transabdominal preperitoneal repair has known benefits, its adoption remains limited due to technical challenges and a steep learning curve. The robotic platform addresses these limitations, making it well-suited for safe, precise dissection in the preperitoneal space. This article presents a practical, step-by-step guide to R-TAPP, highlighting key anatomical landmarks, standardized dissection techniques, and tension-free mesh placement without fixation.
-
Keywords: Inguinal hernia, Robotic surgical procedures, Herniorrhaphy, Minimally invasive surgical procedures
Introduction
Inguinal hernia repair is one of the most common surgeries worldwide, with millions performed annually [1]. Surgical approaches have evolved from open techniques to minimally invasive methods like transabdominal preperitoneal and totally-extraperitoneal repair, which offer benefits such as less postoperative pain, faster recovery, and better cosmetic results [2]. However, widespread adoption of laparoscopic repair remains limited due to a steep learning curve, unfamiliar anatomy, and technical challenges like intracorporeal suturing [3].
Robotic-assisted surgery has emerged as a promising solution, offering enhanced three-dimensional (3D) visualization, wristed instruments for better dexterity, and improved ergonomics—particularly beneficial in the confined preperitoneal space [4]. These advantages make robotic platforms well-suited for inguinal hernia repair.
Recent studies confirm the safety and feasibility of robotic inguinal hernia repair, with outcomes comparable or superior to conventional laparoscopy [3]. Despite concerns over cost and operative time, the robotic approach may offer better precision and a shorter learning curve for selected surgeons [5,6]. This article provides a practical, step-by-step guide to robotic transabdominal preperitoneal (R-TAPP) repair, focusing on key anatomical landmarks and technical strategies to improve surgical outcomes.
Case Presentation
Patient
A 66-year-old man presented with a right inguinal mass noted one month prior. He had a history of gastric perforation in 2020, treated conservatively, and was not on medication. His body mass index was 23.4 kg/m2, and preoperative labs were normal. Computed tomography showed a right indirect inguinal hernia with preperitoneal fat. After discussing options, the patient chose robotic repair, and a right-sided R-TAPP was planned. This study was approved by the Institutional Review Board of National Health Insurance Ilsan Hospital (NHIMC2025-04-003). Written informed consent was waived because of the retrospective nature of the study.
Patient positioning and preparation
Surgical procedure video is edited and presented (video). Patients were placed supine with a 15° Trendelenburg tilt and arms tucked. After general anesthesia, a Foley catheter was inserted if needed. The surgical field was prepped from the subxiphoid area to the proximal thighs for adequate exposure.
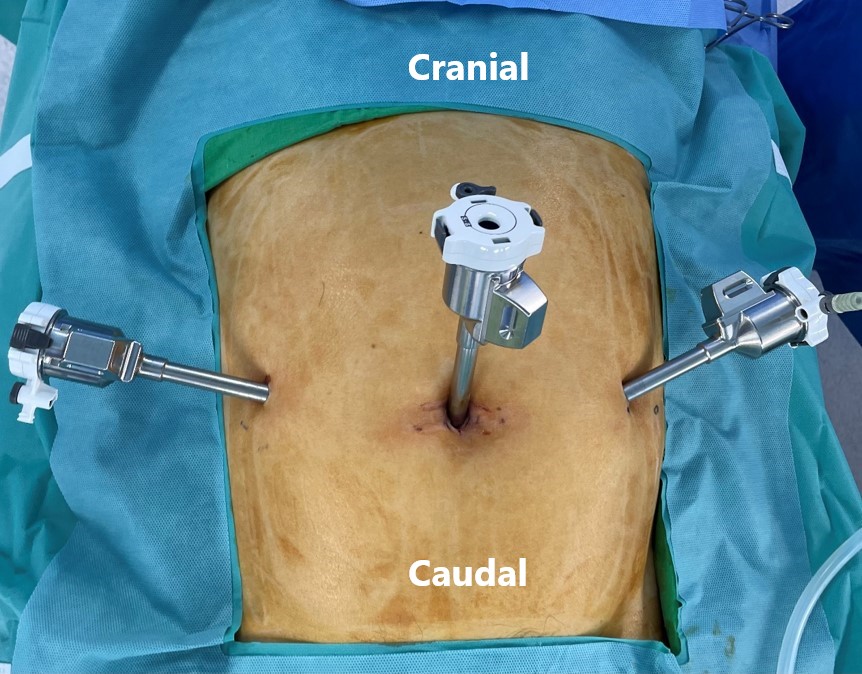
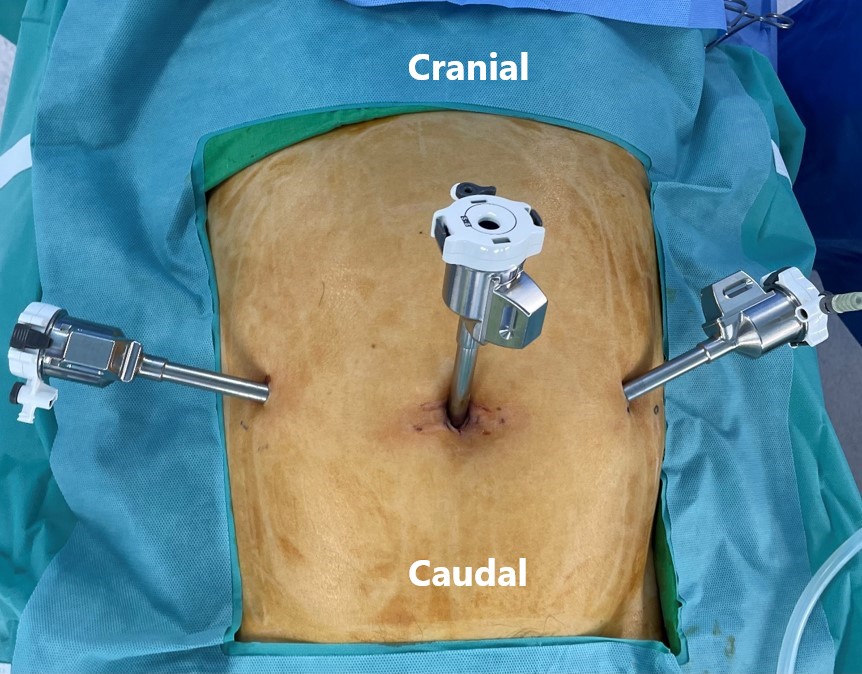
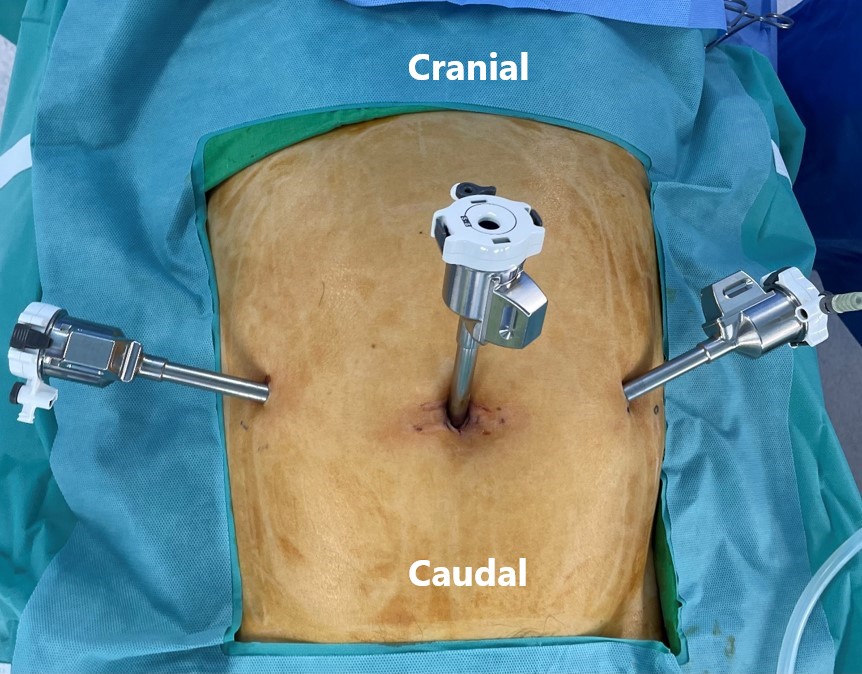
Port placement and docking
A three-port technique is used. An 8 mm optical trocar is inserted at the umbilicus via open technique, with pneumoperitoneum set at 12 mmHg (Fig. 1). Two additional 8 mm trocars are placed under direct vision, about 10 cm from the camera port. The da Vinci Xi system is docked from the patient's right side, and a 30-degree camera provides a wide view of the lower abdomen (Fig. 2).
Peritoneal incision and exposure
A peritoneal incision is made 3–4 cm above the hernia defect, from the medial umbilical ligament to the anterior superior iliac spine, providing space for mesh placement and flap closure. The preperitoneal space is developed with blunt and sharp dissection, preserving key structures like the inferior epigastric vessels and vas deferens or round ligament.
Hernia sac reduction and dissection
For indirect hernias, the sac is separated from the cord structures and reduced toward the internal ring. In direct hernias, the transversalis fascia is reinforced, and redundant sac contents are reduced. Large lipomas or sliding components are thoroughly dissected to minimize recurrence risk. In this case, the patient had a lateral hernia classified as L1 according to the European Hernia Society (EHS) classification, with a defect size of 1.5 cm or less.
Mesh placement
After confirming the absence of occult hernias, a pre-shaped 3DMaxTM mesh (15×10 cm; Bard Davol Inc.) was inserted through the 8 mm port. The mesh was carefully positioned to wrap around the spermatic cord and cover all hernia-prone areas—direct, indirect, and femoral. No fixation was needed, as the mesh’s contour and surrounding anatomy secured it in place. It was laid tension-free, extending from the pubic symphysis to beyond the anterior superior iliac spine, ensuring full coverage without folding or migration.
Peritoneal closure
The peritoneal flap is reapproximated using a running 4-0 absorbable barbed suture in a continuous fashion. Tension-free closure is essential to prevent mesh exposure to intra-abdominal contents, which may increase the risk of adhesions or erosion.
Final Inspection and desufflation
After ensuring hemostasis and confirming mesh position and flap integrity, pneumoperitoneum is reduced. The robotic instruments and ports are removed under direct visualization, and the fascial defect at the camera port. Skin incisions are closed with absorbable sutures or skin adhesive.
Discussion
R-TAPP inguinal hernia repair offers improved dexterity, ergonomics, and visualization over conventional laparoscopy [1]. Although laparoscopic TAPP provides benefits like less pain and quicker recovery, its adoption is limited by technical challenges such as intracorporeal suturing and a steep learning curve, especially for posterior groin anatomy [2,7]. The robotic platform mitigates many of these challenges by offering wristed instrumentation, a stable 3D magnified view, and a more intuitive control system [4]. These features facilitate precise dissection in the preperitoneal space and meticulous peritoneal flap closure, which is often a limiting step in laparoscopic TAPP [2,4]. As noted in recent Korean studies and international literature, R-TAPP has demonstrated safety and feasibility in both primary and complex hernias, with acceptable short-term outcomes and low complication rates [8].
Moreover, robotic hernia repair appears to offer a faster learning curve compared to laparoscopic techniques [5]. Studies suggest that surgical proficiency may be achieved within 20–35 cases depending on prior robotic experience, compared to significantly more cases required for laparoscopic mastery [6]. This technical accessibility, especially for surgeons already trained in robotic platforms, is a significant driver of its increasing adoption.
However, R-TAPP is not without limitations. Increased operative time, particularly in early cases, and higher costs compared to laparoscopic or open techniques remain areas of concern [3]. Nonetheless, emerging data—including meta-analyses—show that robotic repairs may yield lower recurrence rates and improved perioperative outcomes in select populations, particularly in complex or recurrent cases [9].
Finally, it is worth noting that robotic hernia surgery is primarily performed by specialized surgeons, with limited exposure for trainees [10]. As robotic systems become more integrated into surgical training programs, developing structured educational pathways will be essential to ensure broader, safe adoption of this technique.
In conclusion, R-TAPP represents a valuable addition to the surgical armamentarium for inguinal hernia repair. It combines the benefits of minimally invasive surgery with enhanced surgical control and precision. With appropriate case selection, standardized technique, and structured training, R-TAPP has the potential to become a standard approach for inguinal hernia repair in the modern era.
Disclosure
No potential conflict of interest relevant to this article was reported.
Author contributions
Conceptualization: HSL; Writing–original draft: SJ, HSL; Writing–review & editing: SJ, HSL.
Figure 1.Port placement in robotic transabdominal preperitoneal repair.
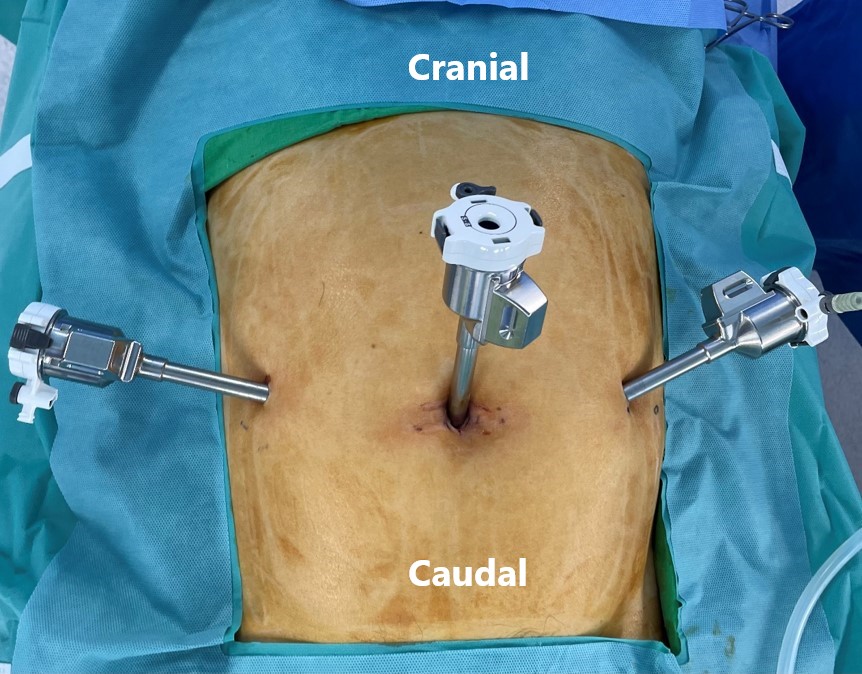
Figure 2.Da Vinci Xi docked with three active arms.

REFERENCES
- 1. de’Angelis N, Schena CA, Moszkowicz D, Kuperas C, Fara R, Gaujoux S, et al. Robotic surgery for inguinal and ventral hernia repair: a systematic review and meta-analysis. Surg Endosc. 2024;38:24-46.ArticlePubMedPDF
- 2. Claus C, Furtado M, Malcher F, Cavazzola LT, Felix E. Ten golden rules for a safe MIS inguinal hernia repair using a new anatomical concept as a guide. Surg Endosc. 2020;34:1458-1464.ArticlePubMedPDF
- 3. Miller BT, Prabhu AS, Petro CC, Beffa LRA, Carbonell AM, Hope W, et al. Laparoscopic versus robotic inguinal hernia repair: 1- and 2-year outcomes from the RIVAL trial. Surg Endosc. 2023;37:723-728.ArticlePubMedPDF
- 4. Jung S, Lee JH, Lee HS. Early outcomes of robotic transabdominal preperitoneal inguinal hernia repair: a retrospective single-institution study in Korea. J Minim Invasive Surg. 2023;26:128-133.ArticlePubMedPMC
- 5. Ephraim K, Haggai B, Mohammad A, Dan A, Yehonatan N, Lior S, et al. Learning curve of robotic inguinal hernia repair in the hands of an experienced laparoscopic surgeon: a comparative study. J Robot Surg. 2022;16:1307-1312.ArticlePubMedPDF
- 6. Solaini L, Cavaliere D, Rocco G, Avanzolini A, Di Pietrantonio D, Ercolani G. Differences in the learning curve of robotic transabdominal preperitoneal inguinal hernia repair according to surgeon’s robotic experience. Hernia. 2023;27:1123-1129.ArticlePubMedPMCPDF
- 7. Choi SI. The feasibility of robotic inguinal henia repair in Korea. J Minim Invasive Surg. 2023;26:108-109.ArticlePubMedPMC
- 8. Varvoglis DN, Sanchez-Casalongue M, Olson MA, DeAngelo N, Garbarine I, Lipman J, et al. Comparison of post-operative outcomes of large direct inguinal hernia repairs based on operative approach (open vs. laparoscopic vs. robotic) using the ACHQC (Abdominal Core Health Quality Collaborative) database. Surg Endosc. 2023;37:2923-2931.ArticlePubMedPDF
- 9. Kudsi OY, Bou-Ayash N, Kaoukabani G, Gokcal F. Comparison of perioperative and mid-term outcomes between laparoscopic and robotic inguinal hernia repair. Surg Endosc. 2023;37:1508-1514.ArticlePubMedPDF
- 10. Hansen DL, Gram-Hanssen A, Fonnes S, Rosenberg J. Robot-assisted groin hernia repair is primarily performed by specialized surgeons: a scoping review. J Robot Surg. 2023;17:291-301.ArticlePubMedPDF
Citations
Citations to this article as recorded by

- Da Vinci Xi versus laparoscopic transabdominal preperitoneal (TAPP) repair of inguinal hernia: a GRADE-assessed systematic review and meta-analysis of randomized controlled trials
Wajahat Mirza, Mehak Ejaz Khan, Hania Iqbal, Alishbah Khan, Hadi Mohammad Khan, Hamza Nasir Chatha, Eshan Ahmad, Sundus Dadan, Abdul Rafeh Awan, Muhammad Ahmad Nadeem
Journal of Robotic Surgery.2025;[Epub] CrossRef
 , Hyung Soon Lee
, Hyung Soon Lee


 PubReader
PubReader ePub Link
ePub Link Cite this Article
Cite this Article

 KSSSG
KSSSG