How to Perform Single-Incision Laparoscopic Totally Extraperitoneal Hernia Repair
Article information
Abstract
Surgery for inguinal hernia has made significant progress over a period of more than a century. The advent of minimally invasive techniques prompted further innovations. Among these, single-incision surgery offers significant advantages in creating the preperitoneal space. Therefore, it is essential for surgeons to understand and be able to perform single-incision laparoscopic totally extraperitoneal (SIL-TEP) hernia repair. This article presents a detailed description of the surgical technique for SIL-TEP.
Introduction
Since tension-free hernia repair using mesh became the gold standard procedure for inguinal hernia surgery [1], there have been numerous advancements in inguinal hernia surgery. The most significant advancement is the application of laparoscopy to the posterior approach [2]. Compared to anterior approaches like Lichtenstein’s tension-free hernioplasty, posterior approaches such as laparoscopic totally extraperitoneal (TEP) or transabdominal preperitoneal (TAPP) hernia repair offer the following advantages: (1) clearer identification of anatomical structures and the hernia with minimal ambiguity, and (2) the ability to use a large mesh that sufficiently covers the entire myopectineal orifice.
Although relatively high technical difficulty of single incision laparoscopic surgery has limited its widespread adoption, there is a consensus among many hernia surgeons regarding the efficiency and safety of the technique, supported by research findings [3-5].
Case Presentation
Patient
The patient is a 64-year-old male with a 6-month history of right inguinal hernia. A reducible soft mass, approximately 3×3 cm, was observed in the right inguinal region. In typical cases, no specific imaging tests are required for inguinal hernia, and diagnosis based on physical examination is sufficient. This study was approved by the Institutional Review Board of Incheon St. Mary’s Hospital (approval number: OC25ZASI0061). Informed consent was waived due to the retrospective study design and use of anonymized data.
Surgical procedure of single-incision laparoscopic totally extraperitoneal hernia repair
Skin incision
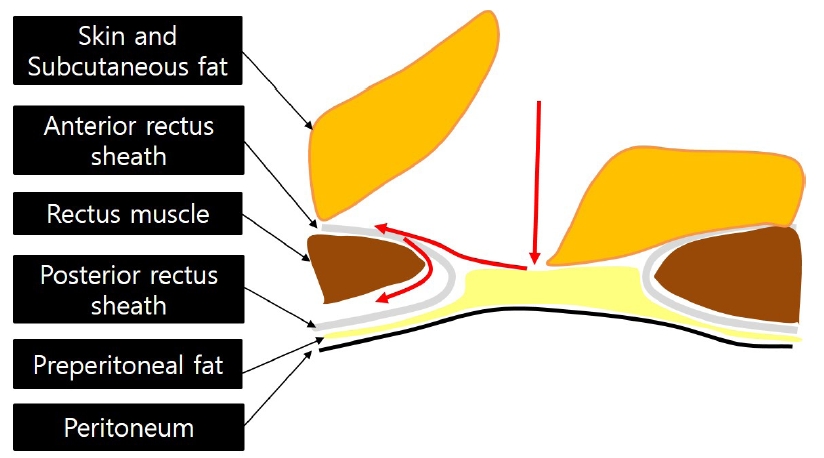
A 2–2.5 cm trans-umbilical skin incision is typically used. The trans-umbilical incision is chosen to minimize scarring, but any incision providing access to the retro-rectus space is acceptable. When using a trans-umbilical incision, a subcutaneous flap is created along the anterior rectus sheath toward the hernia site after the skin incision. Then, the anterior rectus sheath is incised, the rectus muscle is identified, and a wound protector is inserted between the rectus muscle and posterior rectus sheath (Fig. 1).
Fundamental technique of single-incision laparoscopic surgery
Proper positioning of the laparoscope and two working instruments within the single-port platform is essential. As illustrated in Fig. 2A, the laparoscope should be placed centrally within the single-port platform, with the left-hand instrument inserted to the left of the scope and the right-hand instrument inserted to the right of the scope, both passing through the umbilicus into the abdominal cavity. However, as shown in Fig. 2B, the instruments should not be crossed within the single-port platform (i.e., prior to transumbilical entry), as this significantly limits the range of motion of the instruments. It is acceptable for the instruments to cross after entering the abdominal cavity (Fig. 2C).
Intraperitoneal procedure (video)
(1) Step 1. Space making (preperitoneal space dissection)
Surgery is performed using a 5 mm rigid, 30-degree long scope and conventional straight instruments. The extent of space creation should include identification of the symphysis pubis medially and extend laterally beyond the level of the anterior superior iliac spine. Inferiorly, dissection should reach the space of Retzius, and inferolaterally, it should extend to the psoas muscle and Bogros space. The most critical anatomical landmarks in this process are the inferior epigastric vessels and pubic bone.
The video shows multiple small communicating vessels between the posterior rectus sheath and rectus muscle, which can be managed without bleeding using coagulation under direct vision. The video also shows the arcuate line and transversalis fascia below it. The transversalis fascia typically tears naturally, allowing access to the preperitoneal space. In the space of Retzius on the medial side of the spermatic cord, dissection should be performed just above the preperitoneal fat. In the space of Bogros on the lateral side of the spermatic cord, dissection should be performed just below the preperitoneal fat (immediately above the peritoneum).
(2) Step 2. Identify the anatomy and hernia
The following structures must be identified during surgery: inferior epigastric vessels, pubic bone, Cooper’s ligament, spermatic cord, myopectineal orifice, and three hernia sites (deep inguinal ring, Hesselbach’s triangle, femoral ring). While external iliac vessels do not require direct visualization, their location beyond the spermatic cord must be noted.
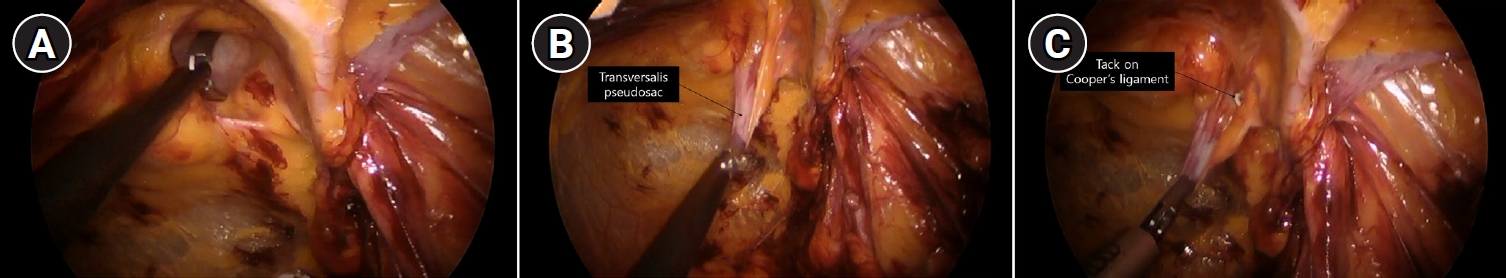
(3) Step 3. Handling of hernia sac
For indirect inguinal hernia, the hernia sac must be separated from the spermatic cord structures using sharp dissection. Within the spermatic cord, the internal spermatic vessels are located on the lateral side, and the ductus deferens is on the medial side. For indirect inguinal hernia, it is not necessary to completely separate the entire hernia sac from the spermatic cord; as shown in the video, it can be divided midway and ligated. However, when the sac is preserved entirely without transection and inverted into the peritoneal cavity, ligation is not necessarily required.
For direct inguinal hernia, the hernia sac consists of preperitoneal fat and peritoneum, appearing as fat, and can be separated from surrounding tissues (transversalis pseudosac) relatively easily using blunt dissection (Fig. 3). For a large direct hernia pseudosac (stretched transversalis fascia), it is recommended to pull and fix it to Cooper’s ligament, although no clear size criteria exist (Fig. 4).
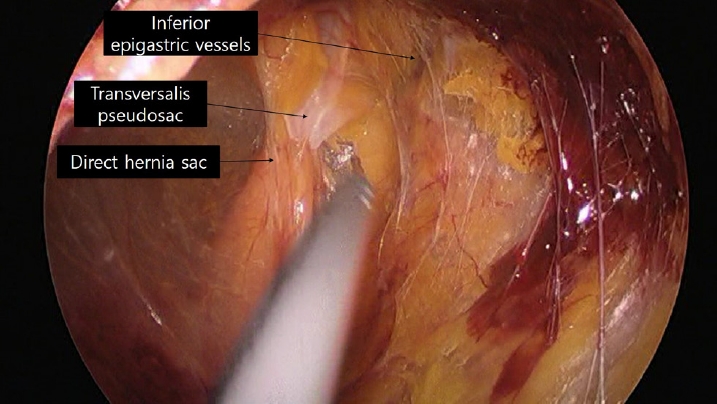
Surgical view of a direct hernia. The outer layer of the hernia sac consists of preperitoneal tissue.
(4) Step 4. Parietalization
This is the most critical step in preventing hernia recurrence. Adequate preperitoneal (space of Retzius) and peritoneal (space of Bogros) dissection ensures the mesh covers the myopectineal orifice (Fig. 5). The extent of parietalization should be determined under the assumption that the mesh is in place, ensuring that an appropriate distance is maintained between the mesh’s inferior margin and the peritoneal reflection. Although no clear guideline exists for the appropriate distance, many experts suggest approximately 2 cm (Fig. 6).
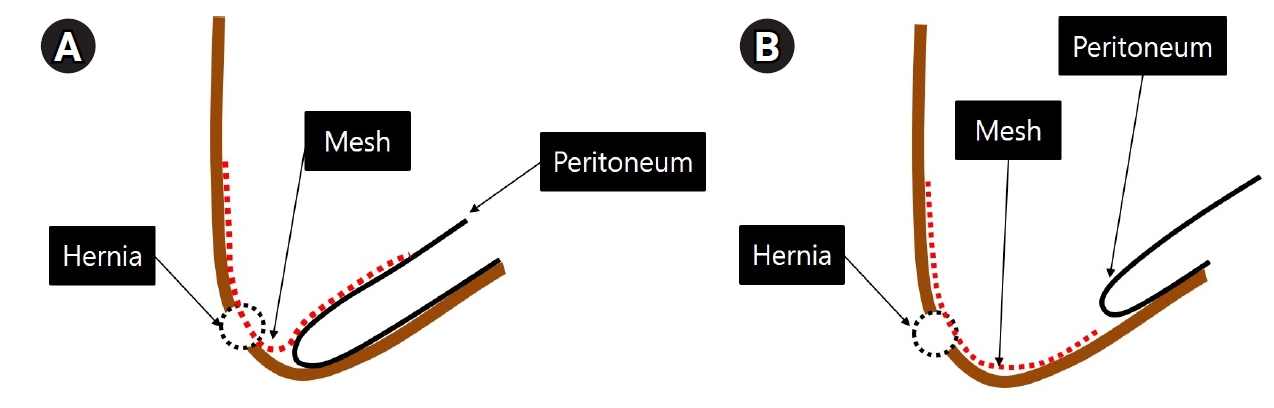
(A) Insufficient parietalization results in mesh folding after surgery. (B) Adequate parietalization ensures the peritoneum naturally covers the mesh without folding.
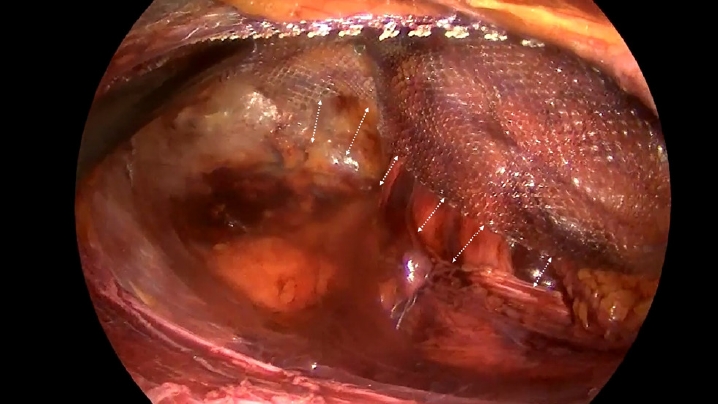
(5) Step 5. Placement of the mesh
A 15-×10-cm mesh is typically recommended. The mesh should cover all fascial defects in the groin without wrinkles, including Hesselbach’s triangle, the deep inguinal ring, and the femoral ring. The use of tacks for mesh fixation is discouraged, and atraumatic mesh fixation (e.g., fibrin glue) is recommended. After placing the mesh in the correct position, the gas is removed from the operative field, ensuring the mesh remains unfolded until the end.
Discussion
Single-incision laparoscopic (SIL)-TEP is a safe and technically feasible surgical method compared to conventional TEP [4,5]. The greatest advantage of SIL-TEP lies in the space-making step among the five surgical steps. The advantage of single-incision laparoscopic surgery is the ability to expand a small space into a larger one. Through the scope and two working instruments, appropriate traction and counter-traction under direct vision enable delicate dissection. This delicate dissection allows surgery to proceed in a more precise surgical plane, referring to surgery through an embryological avascular plane. Less blood contamination in the operative field enhances surgical precision synergistically. Another technical advantage is during mesh placement. The absence of a supra-pubic port facilitates mesh placement in that area.
Although the indications and contraindications for SIL-TEP are identical to those of conventional TEP and TAPP, the procedure is relatively more technically challenging. For beginners, it is advisable to perform the surgery under the supervision of an experienced hernia surgeon. Additionally, accumulating appropriate surgical experience before performing the procedure is crucial. Practice in both single-incision surgery and laparoscopic hernia repair techniques is necessary.
Notes
Disclosure
No potential conflict of interest relevant to this article was reported.
Author contributions
Conceptualization: MJK, JHK, JMS, CDL; Supervision: MJK, JMS; Writing–original draft: MJK; Writing–review & editing: MJK, JHK, JMS, CDL.