High Lymph Node Dissection with Low Ligation: A Modified Technique for Left Colic Artery Preservation in Colorectal Cancer
Article information
Abstract
The optimal level of inferior mesenteric artery (IMA) ligation in colorectal cancer remains controversial. High ligation allows complete D3 lymphadenectomy but sacrifices the left colic artery (LCA), raising concerns about anastomotic ischemia. This report presents a modified low ligation technique that achieves radical D3 dissection while preserving the LCA. The technique involves complete skeletonization of the IMA root with en bloc removal of surrounding lymphatic tissue while maintaining LCA continuity. Key procedural steps include: (1) medial-to-lateral mobilization, (2) exposure of the IMA origin, (3) para-IMA lymph node dissection along the vascular sheath, (4) preservation of the LCA and autonomic plexus, and (5) distal IMA division below the LCA bifurcation. Intraoperative images illustrate the dissected nodal field and preserved vasculature. This technique enables D3-level lymph node dissection comparable to high ligation, with clear visualization of the IMA root and preserved arterial supply. Thirty-five lymph nodes, including one metastatic node, were retrieved without compromising perfusion. This modified approach balances oncologic completeness with physiologic preservation and may serve as a practical model for achieving D3 lymphadenectomy with vascular preservation.
Introduction
The level of inferior mesenteric artery (IMA) ligation in colorectal cancer surgery remains debated. High ligation (HL) at the aortic origin allows extensive D3 dissection and removal of para-IMA nodes [1], but sacrifices the left colic artery (LCA) and may increase anastomotic ischemia [2]. Low ligation (LL) preserves the LCA and physiological blood flow but may result in limited lymph node retrieval at the IMA root [1].
With open surgery and early laparoscopy, exposing the IMA origin while preserving surrounding structures was difficult [3]. Modern high-definition laparoscopy and robotic systems permit precise visualization and safer skeletonization, yet many surgeons still perform HL. This gap underscores the need for approaches that reflect current technological capabilities.
To address this, we developed a modified LL technique that enables complete D3 lymph node dissection while preserving the LCA and autonomic plexus [4].
Case Presentation
Medial-to-lateral mobilization
The peritoneum is incised between the right common iliac artery and the IMA or sigmoid artery to enter the pelvic mesenteric plane. Cranial dissection continues beneath the IMA. The peritoneum along the right border of the inferior mesenteric vein connects upper and lower planes (Fig. 1).
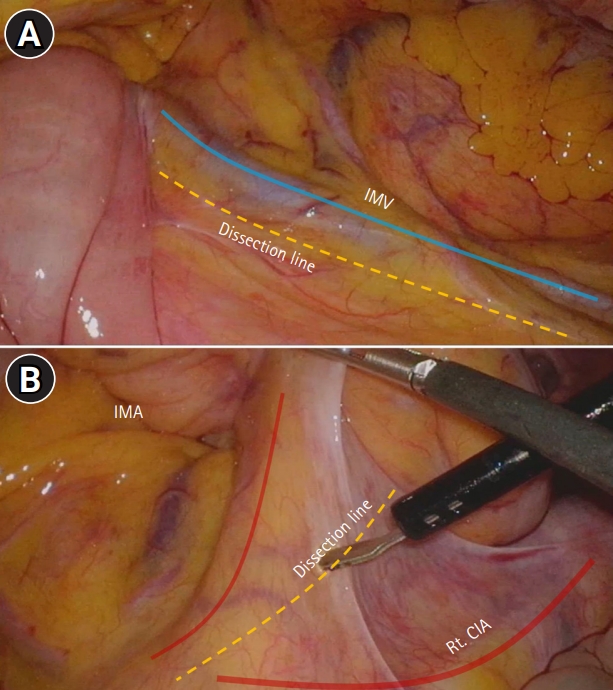
Medial-to-lateral mobilization. (A) The peritoneum along the right (Rt.) border of the inferior mesenteric vein (IMV) is incised to connect the upper and lower planes, creating a continuous medial-to-lateral field. (B) The peritoneum is incised between the Rt. common iliac artery (CIA) and the inferior mesenteric artery (IMA) or sigmoid artery to enter the pelvic mesenteric plane.
Inferior mesenteric artery exposure and nerve preservation
Traction on the mesocolon exposes the IMA origin. The hypogastric plexus and autonomic nerves are preserved by maintaining the dissection anterior to the neural sheath and identifying the ureter and gonadal vessels as the lateral boundary of the safe plane, while the proximal IMA is skeletonized along the vascular sheath.
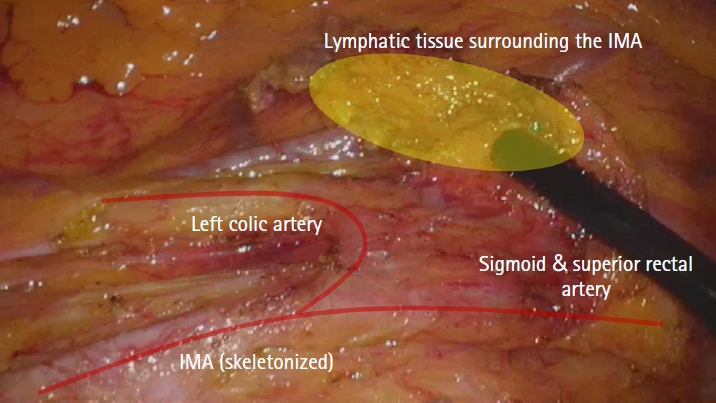
Lymph node dissection
Para-IMA lymphatic tissue is removed en bloc, extending distally for full IMA skeletonization while maintaining a close posterior plane to avoid nerve injury (Fig. 2).
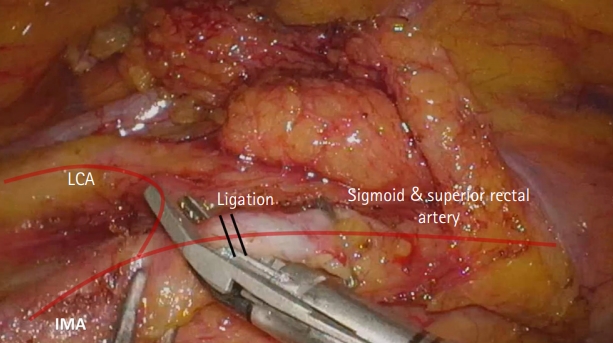
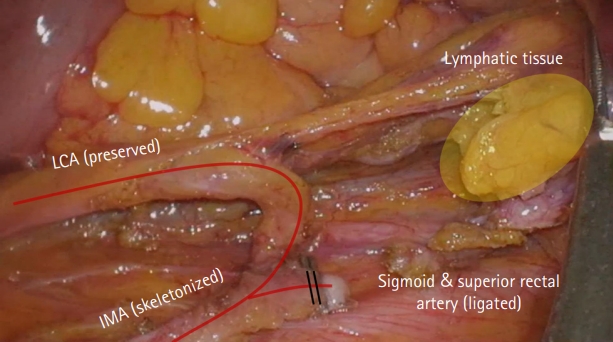
Left colic artery–sigmoid bifurcation and selective ligation
Complete skeletonization exposes the bifurcation. The LCA is preserved; only the sigmoid artery is ligated. Distal lymphatics along the LCA remain with the specimen (Fig. 3).
Mobilization and resection
Lateral mobilization proceeds toward the splenic flexure. The specimen includes sigmoid/upper rectal mesentery and lymphatic tissue from the IMA root to the sigmoid bifurcation (Fig. 4).
Summary
This technique achieves D3 lymphadenectomy while preserving the LCA through sequential skeletonization of the IMA. Thirty-five lymph nodes were retrieved, including one metastatic, comparable to HL. The high lymph node dissection with low ligation (HD-LL) therefore provides radical oncologic clearance while maintaining physiological perfusion.
Ethical approval
This report includes non-identifiable intraoperative images; therefore, institutional review board approval was not required.
Discussion
HL enables thorough lymphadenectomy but sacrifices the LCA, increasing ischemic risk [2], whereas LL preserves blood flow but may limit lymph node clearance [1]. The HD-LL technique addresses this by enabling complete skeletonization of the IMA root and D3 lymphadenectomy while preserving the LCA and autonomic plexus [4,5].
However, preserving the LCA can reduce the mobility of the descending colon and increase anastomotic tension, which represents a practical limitation of LL. In contrast, HL can relieve mesenteric tension and facilitate a tension-free anastomosis, particularly in low rectal cancer where greater colonic reach is required. Therefore, the ligation level should be tailored to the balance between perfusion preservation and mesenteric mobility.
LL may be preferable in patients in whom preserving arterial perfusion is critical, such as those with high anastomotic leak risk. Patients with high anastomotic leak risk—such as those with corticosteroid use, smoking, diabetes, obesity, malnutrition, vascular disease, or prior neoadjuvant chemoradiation—may derive greater advantage from preserving the LCA. Conversely, when mesenteric reach is limited or tension reduction is a priority, HL may be more suitable.
The 35-node yield in our case was comparable to conventional HL [1,4], demonstrating that perfusion can be preserved without compromising oncologic completeness.
Modern laparoscopic and robotic platforms facilitate precise dissection and selective vascular preservation, shifting focus from the “height of ligation” to the “depth of dissection and anatomic precision.” While promising, the technique requires adequate anatomical understanding and technical proficiency. Broader validation through multi-institutional experience will further establish its utility.
Notes
Disclosure
No potential conflict of interest relevant to this article was reported.
Author contributions
Conceptualization: JP, BKP; Data curation: JP, BGK, YGP; Formal analysis: JP; Investigation: JP; Methodology: JP, BGK, YGP; Project administration: BKP; Software: JP; Supervision: BKP; Validation: BGK, YGP; Visualization: JP; Writing–original draft: JP; Writing–review & editing: BGK, YGP, BKP.