Articles
- Page Path
- HOME > J Surg Innov Educ > Volume 2(2); 2025 > Article
-
How I Do It
Laparoscopic Inguinal Hernia Repair in Female Pediatric Patients -
Joong Kee Youn1,2

-
Journal of Surgical Innovation and Education 2025;2(2):35-38.
DOI: https://doi.org/10.69474/jsie.2025.00325
Published online: December 19, 2025
1Department of Pediatric Surgery, Seoul National University Hospital, Seoul, Republic of Korea
2Department of Surgery, Seoul National University College of Medicine, Seoul, Republic of Korea
- Corresponding author: Joong Kee Youn, MD, PhD Department of Pediatric Surgery, Seoul National University Hospital, 101 Daehak-ro, Jongno-gu, Seoul 03080, Republic of Korea Tel: +82-2-2072-4252, Fax: +82-2-747-5130, E-mail: bead47@snu.ac.kr
• Received: November 11, 2025 • Revised: December 10, 2025 • Accepted: December 10, 2025
© 2025 Korean Surgical Skill Study Group
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 0 Views
- 6 Download
Abstract
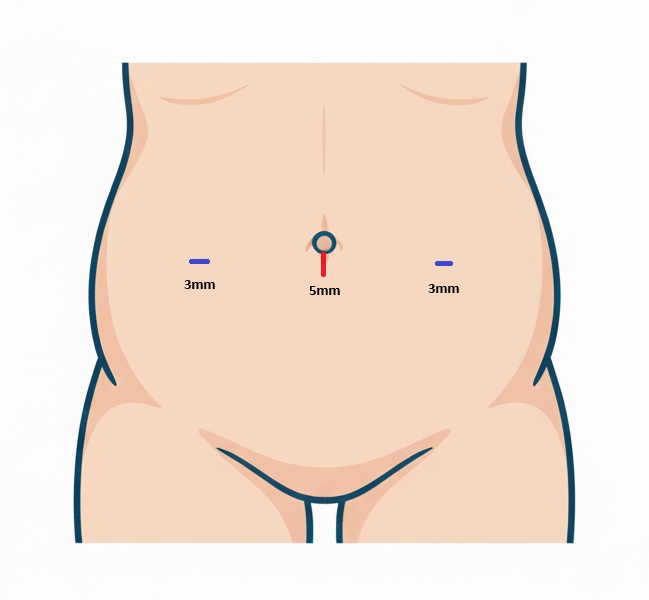
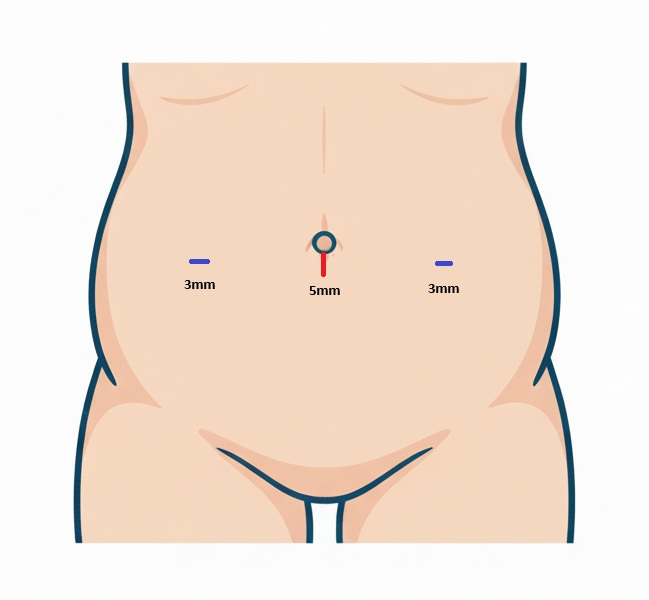
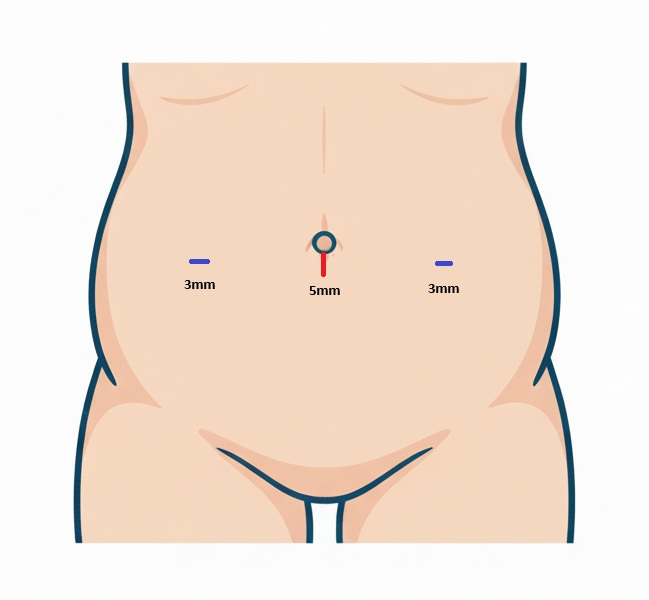
- Laparoscopic inguinal hernia repair (LIHR) has become a widely adopted surgical approach for pediatric inguinal hernia because it offers superior visualization and enables simultaneous assessment of the contralateral side. An 8-month-old female infant presented with a spontaneously reducing bulge in the right inguinal region, most noticeable during diaper changes. Physical examination revealed an easily reducible inguinal mass that was palpably firm and spherical, raising strong suspicion for ovarian inclusion. A positive silk glove sign was also identified on the contralateral side. Under general anesthesia, a three-port laparoscopic technique was used, consisting of a 5-mm umbilical port and two 3-mm working ports. The peritoneum and gubernaculum were carefully dissected from surrounding structures using electrocautery before sac closure, a step performed to minimize the risk of recurrence. Both the symptomatic right hernia sac and the asymptomatic contralateral patent processus vaginalis, which was visually confirmed intraoperatively, were closed using an intracorporeal purse-string high ligation with absorbable sutures. Three-port LIHR with meticulous dissection of the peritoneum and gubernaculum represents an effective and definitive technique for pediatric inguinal hernia repair. This approach allows simultaneous bilateral repair and is associated with excellent postoperative recovery, supporting its continued use as a primary surgical method.
Introduction
Case Presentation
Discussion
Fig. 1.The size and position of laparoscopic ports applied in pediatric laparoscopic inguinal hernia repair.
- 1. Chang SJ, Chen JY, Hsu CK, Chuang FC, Yang SS. The incidence of inguinal hernia and associated risk factors of incarceration in pediatric inguinal hernia: a nation-wide longitudinal population-based study. Hernia. 2016;20:559-563.ArticlePubMedPDF
- 2. Esposito C, Montupet P. Laparoscopic treatment of recurrent inguinal hernia in children. Pediatr Surg Int. 1998;14:182-184.ArticlePubMed
- 3. Gorsler CM, Schier F. Laparoscopic herniorrhaphy in children. Surg Endosc. 2003;17:571-573.ArticlePubMedPDF
- 4. Ostlie DJ, Ponsky TA. Technical options of the laparoscopic pediatric inguinal hernia repair. J Laparoendosc Adv Surg Tech A. 2014;24:194-198.ArticlePubMed
- 5. Oue T, Kubota A, Okuyama H, Kawahara H. Laparoscopic percutaneous extraperitoneal closure (LPEC) method for the exploration and treatment of inguinal hernia in girls. Pediatr Surg Int. 2005;21:964-968.ArticlePubMedPDF
- 6. Shalaby R, Ismail M, Dorgham A, Hefny K, Alsaied G, Gabr K, et al. Laparoscopic hernia repair in infancy and childhood: evaluation of 2 different techniques. J Pediatr Surg. 2010;45:2210-2216.ArticlePubMed
- 7. Esposito C, Escolino M, Cortese G, Aprea G, Turrà F, Farina A, et al. Twenty-year experience with laparoscopic inguinal hernia repair in infants and children: considerations and results on 1833 hernia repairs. Surg Endosc. 2017;31:1461-1468.ArticlePubMedPDF
- 8. Muta Y, Odaka A, Inoue S, Takeuchi Y, Beck Y. Female pediatric inguinal hernia: uterine deviation toward the hernia side. Pediatr Surg Int. 2021;37:1569-1574.ArticlePubMedPDF
- 9. Oshiba A, Ashour K, Aboheba M, Shehata S, Shalaby R. Comparative study between purse–string suture and peritoneal disconnection with ligation techniques in the laparoscopic repair of inguinal hernia in infants and children. Ann Pediatr Surg. 2016;12:137-141.Article
- 10. Boo YJ, Han HJ, Ji WB, Lee JS. Laparoscopic hernia sac transection and intracorporeal ligation show very low recurrence rate in pediatric inguinal hernia. J Laparoendosc Adv Surg Tech A. 2012;22:720-723.ArticlePubMed
REFERENCES
Figure & Data
References
Citations
Citations to this article as recorded by 

 PubReader
PubReader ePub Link
ePub Link-
 Cite this Article
Cite this Article
- Cite this Article
-
- Close
- Download Citation
- Close
- Figure
Laparoscopic Inguinal Hernia Repair in Female Pediatric Patients
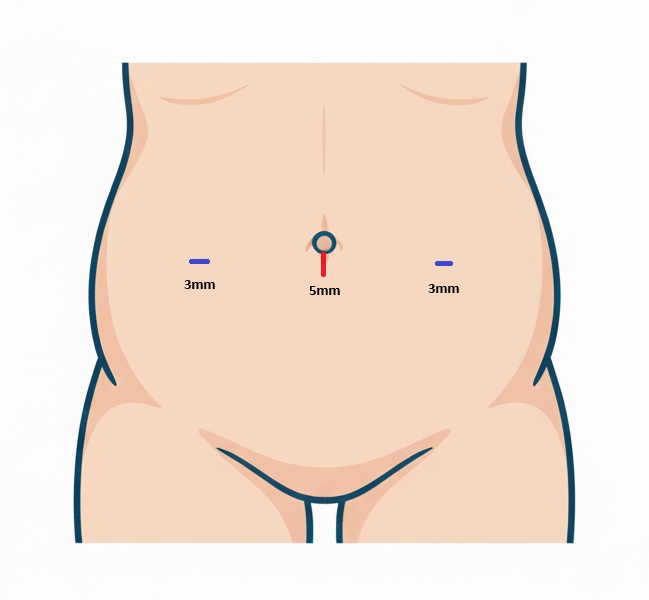
Fig. 1. The size and position of laparoscopic ports applied in pediatric laparoscopic inguinal hernia repair.
Fig. 1.
Laparoscopic Inguinal Hernia Repair in Female Pediatric Patients
TOP
 KSSSG
KSSSG