Articles
- Page Path
- HOME > J Surg Innov Educ > Volume 1(1); 2024 > Article
-
How I Do It
How I Do It: The Very First Laparoscopic Cholecystectomy as a First-Year Resident, with a Step-by-Step Tutorial -
Sujin Park
 , Hochang Chae
, Hochang Chae , Hyeong Seok Kim
, Hyeong Seok Kim , Hongbeom Kim
, Hongbeom Kim , Sang Hyun Shin
, Sang Hyun Shin , In Woong Han
, In Woong Han , Jin Seok Heo
, Jin Seok Heo , So Jeong Yoon
, So Jeong Yoon
-
Journal of Surgical Innovation and Education 2024;1(1):10-13.
DOI: https://doi.org/10.69474/jsie.2024.00024
Published online: June 25, 2024
Division of Hepatobiliary-Pancreatic Surgery, Department of Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Republic of Korea
- Corresponding author: So Jeong Yoon, MD, PhD Division of Hepatobiliary-Pancreatic Surgery, Department of Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, 81 Irwon-ro, Gangnam-gu, Seoul 06351, Republic of Korea Tel: +82-2-3410-0772, E-mail: wooyabi@gmail.com
© 2024 Korean Surgical Skill Study Group
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (https://creativecommons.org/licenses/by-nc/4.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 46 Views
- 22 Download
Abstract
- Since its introduction in 1987, laparoscopic cholecystectomy (LC) has been widely performed by surgeons as a standard procedure for benign gallbladder diseases. Education and training by hepatobiliary experts are important in order to safely perform LC without critical complications. The present report discusses the first LC performed by a beginner surgeon who was trained with our institutional step-by-step tutorial. The step-by-step mentor-mentee tutorial had a total of four phases: video training, observation in the operating room, participation as an assistant, and finally performing LC independently. At every step, the mentor’s approval was required to move on to the next phase. After completing visual training and observation, the mentee participated in 10 consecutive LCs as an assistant or operator. Finally, LC for a 54-year-old female patient with gallbladder stones was independently performed by the mentee under the mentor’s supervision. The patient was discharged on the first postoperative day without complications. We report a case of LC successfully performed by a beginner surgeon with the aid of a newly established step-by-step tutorial. The tutorial is expected to be applied to numerous surgical trainees after further refinement regarding its safety and feasibility.
Introduction
Case Presentation
Results
Discussion
Disclosure
No potential conflict of interest relevant to this article was reported.
Funding
This research was supported by a grant (grant number: HI20C1234) of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea.
Author contributions
Conceptualization: SP, SJY; Data curation: SP, HC, HSK, SJY; Formal analysis: SP, HC, HSK, HK, SHS, IWH, JSH, SJY; Investigation: SP, HC, HSK, HK, SHS, IWH, JSH, SJY; Methodology: SP, SJY; Funding acquisition: SJY, IWH; Writing–original draft: SP, HC, HSK, HK, SHS, IWH, JSH, SJY; Writing–review & editing: SP, HC, HSK, HK, SHS, IWH, JSH, SJY.
- 1. Wang X, Yu W, Jiang G, Li H, Li S, Xie L, et al. Global epidemiology of gallstones in the 21st century: a systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2024 Feb 19 [Epub]. DOI: 10.1016/j.cgh.2024.01.051.ArticlePubMed
- 2. Riddell ZC, Corallo C, Albazaz R, Foley KG. Gallbladder polyps and adenomyomatosis. Br J Radiol. 2023;96:20220115.ArticlePubMedPMC
- 3. Csikesz NG, Singla A, Murphy MM, Tseng JF, Shah SA. Surgeon volume metrics in laparoscopic cholecystectomy. Dig Dis Sci. 2010;55:2398-2405.ArticlePubMedPDF
- 4. Jung YK, Kwon YJ, Choi D, Lee KG. What is the safe training to educate the laparoscopic cholecystectomy for surgical residents in early learning curve? J Minim Invasive Surg. 2016;19:70-74.Article
- 5. Lim SH, Salleh I, Poh BK, Tay KH. Laparoscopic cholecystectomy: an audit of our training programme. ANZ J Surg. 2005;75:231-233.ArticlePubMed
- 6. Jung YK, Choi D, Lee KG. Learning laparoscopic cholecystectomy: a surgical resident’s insight on safety and training during the initial 151 cases. Indian J Surg. 2021;83:224-229.ArticlePDF
- 7. Bresadola V, Pravisani R, Pighin M, Seriau L, Cherchi V, Giuseppe S, et al. Clinical strategies to aim an adequate safety profile for patients and effective training for surgical residents: the laparoscopic cholecystectomy model. Ann Med Surg (Lond). 2016;11:58-61.ArticlePubMedPMC
- 8. Wong HJ, Kojima Y, Su B, Attaar M, Wu H, Campbell M, et al. Long-term retention after structured curriculum on attainment of critical view of safety during laparoscopic cholecystectomy for surgeons. Surgery. 2022;171:577-583.ArticlePubMed
REFERENCES
Figure & Data
References
Citations

 PubReader
PubReader ePub Link
ePub Link-
 Cite this Article
Cite this Article
- Cite this Article
-
- Close
- Download Citation
- Close
- Figure

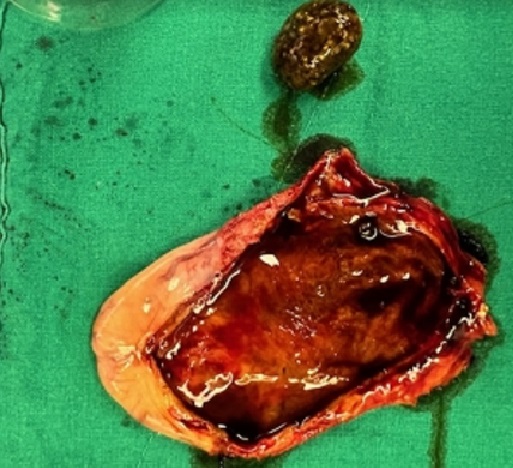
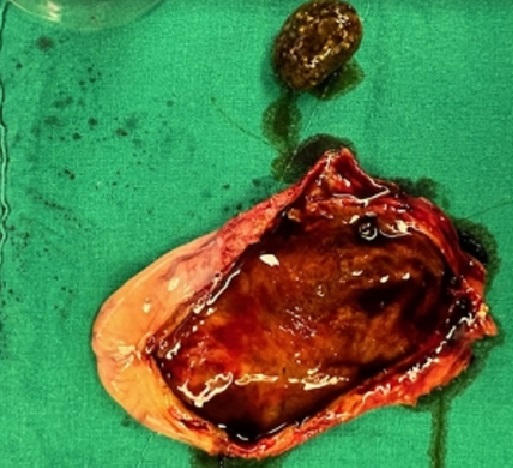
Figure 1.
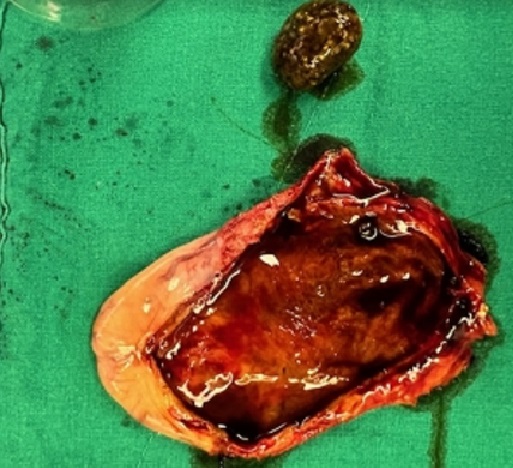
Figure 2.
| Phase | Detail | Duration/Requirement |
|---|---|---|
| 1st: video training | - Understanding biliary anatomy | At least 2 weeks/A case review note |
| - Learning the details of LC | ||
| 2nd: observation | - Observing a mentor performing LC in the operating room | At least 1 week/5 cases recommended |
| - Questions and answers in real time | ||
| 3rd: participation | - A stepwise approach (checklist: proceeding to the next step only after obtaining confirmation from the supervisor) | At least 1 week/At least 2 tries fully completed by a mentee |
| a. Incision and trocar insertion | ||
| b. Recognition of anatomy: bile duct and Calot’s triangle | ||
| c. Dissection of Calot’s triangle and achieving the “critical view of safety” | ||
| d. Ligation of cystic duct and cystic artery | ||
| e. Dissection of gallbladder from liver bed (troubleshooting tips: a “top-down” technique) | ||
| f. Bleeding control and specimen removal | ||
| g. Closing trocar sites | ||
| 4th: operation | - Performing LC under the supervision of a mentor | - |
LC, laparoscopic cholecystectomy.
Table 1.
TOP
 KSSSG
KSSSG