Articles
- Page Path
- HOME > J Surg Innov Educ > Volume 1(1); 2024 > Article
-
How I Do It
Techniques in Jejunojejunostomy, Gastrojejunostomy, and Esophagojejunostomy in Reduced-Port Gastrectomy -
Sa-Hong Min

-
Journal of Surgical Innovation and Education 2024;1(1):3-5.
DOI: https://doi.org/10.69474/jsie.2024.00031
Published online: June 25, 2024
Department of Gastrointestinal Surgery, Asan Medical Center, Seoul, Republic of Korea
- Corresponding author: Sa-Hong Min, MD Department of Gastrointestinal Surgery, Asan Medical Center, 88 Olympic-ro 43-gil, Songpa-gu, Seoul 05505, Republic of Korea Tel: +82-2-3010-3421, SE-mail: shmin823@gmail.com
• Received: May 27, 2024 • Revised: June 13, 2024 • Accepted: June 17, 2024
© 2024 Korean Surgical Skill Study Group
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (https://creativecommons.org/licenses/by-nc/4.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 52 Views
- 34 Download
Abstract
- Minimally invasive gastric cancer surgery aims to reduce morbidity and mortality while maintaining satisfactory oncological outcomes. Laparoscopic gastrectomy is a standard treatment, offering reduced pain, shorter hospital stays, and faster recovery. Reduced-port gastrectomy has gained popularity due to its requirement for limited assistants; however, it poses unique challenges. This paper shares the techniques used in three cases of jejunojejunostomy, gastrojejunostomy, and esophagojejunostomy during reduced-port gastrectomy. Reduced-port techniques were successfully implemented in all three cases. Key steps included proper port placement, the use of tagging sutures, and strategic stapler insertion and adjustment. The reduced-port approach demonstrated feasibility and effectiveness despite its inherent challenges. Reduced-port gastrectomy can be effectively performed with a careful technique and meticulous planning, despite the challenges of transitioning from conventional five-port techniques. Using fewer ports results in less pain, fewer complications, and shorter hospital stays without compromising oncologic outcomes. These techniques can be helpful for trainees and novice surgeons, though careful candidate selection is paramount.
Introduction
Case Presentation
Discussion
Disclosure
Sa-Hong Min is an associate editor of the journal, but he was not involved in the peer reviewer selection, evaluation, or decision process of this article. No other potential conflicts of interest relevant to this article were reported.
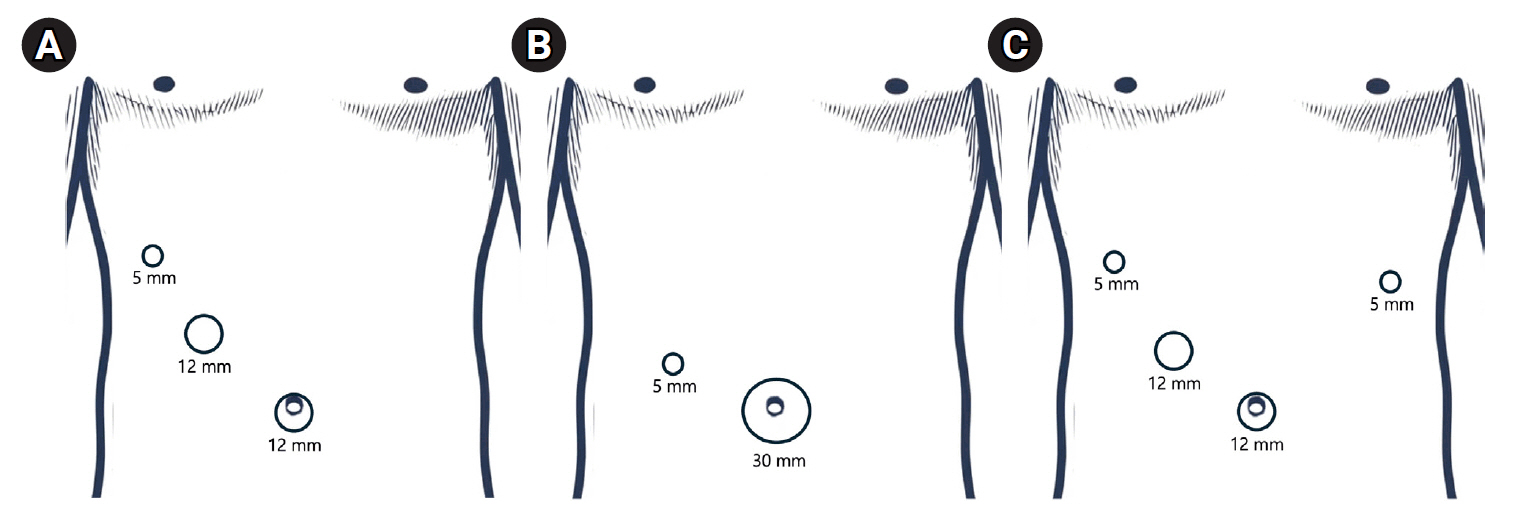
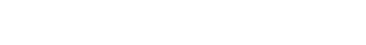
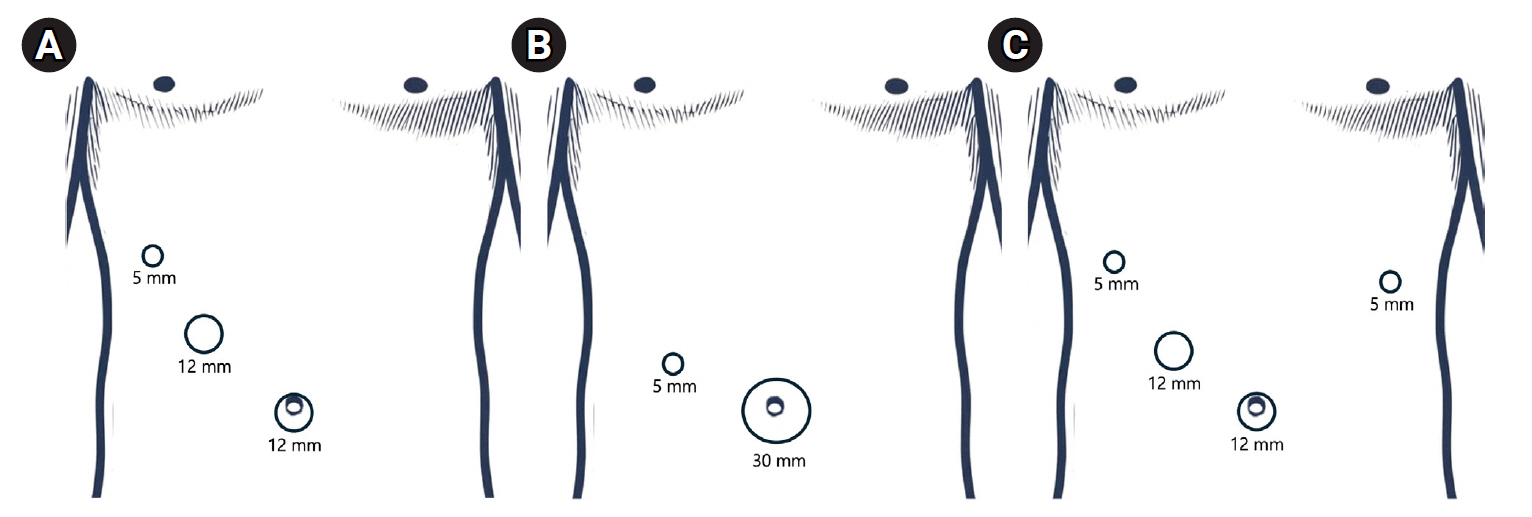
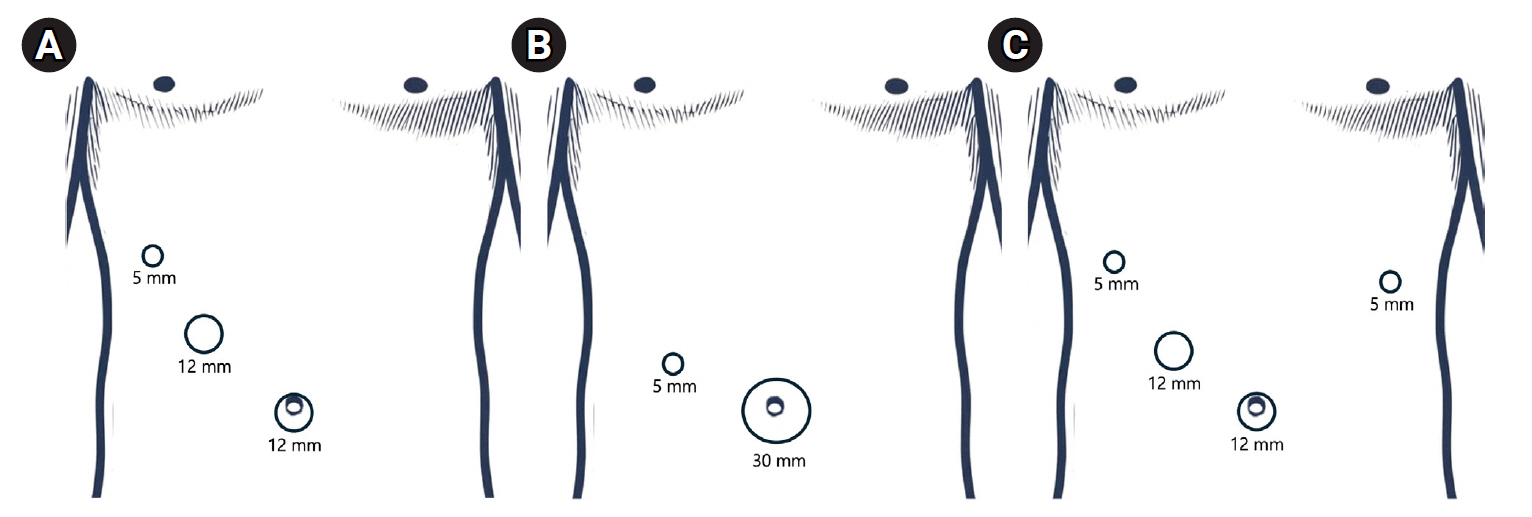
Figure 1.Laparoscopic port placements for the three cases. (A) Three-port surgery, (B) 2-port surgery, (C) 4-port surgery.
- 1. Kim JW. Current issues in reduced-port gastrectomy: a comprehensive review. J Gastric Cancer. 2024;24:57-68.ArticlePubMedPMCPDF
- 2. Kim TH, Kim IH, Kang SJ, Choi M, Kim BH, Eom BW, et al. Korean practice guidelines for gastric cancer 2022: an evidence-based, multidisciplinary approach. J Gastric Cancer. 2023;23:3-106.ArticlePubMedPMC
- 3. Inaki N, Tsuji T, Doden K, Sakimura Y, Tawara H, Matsui R, et al. Reduced port laparoscopic gastrectomy for gastric cancer. Transl Gastroenterol Hepatol. 2016;1:38.ArticlePubMedPMC
- 4. Kim HG, Kim DY, Jeong O. Transition from conventional to reduced-port laparoscopic gastrectomy to treat gastric carcinoma: a single surgeon’s experience from a small-volume center. J Gastric Cancer. 2018;18:172-181.ArticlePubMedPMCPDF
- 5. Lee HH, Jeong O, Seo HS, Choi MG, Ryu SY, Sohn TS, et al. Long-term oncological outcomes of reduced three-port laparoscopic gastrectomy for early-stage gastric carcinoma: a retrospective large-scale multi-institutional study. J Gastric Cancer. 2021;21:93-102.ArticlePubMedPMCPDF
- 6. Lin L, Xu Q, Xu F, Zhou C, Huang X, Chen R, et al. Comparison of short-term surgical outcomes and post-operative recovery between single-incision and multi-port laparoscopic distal gastrectomy for gastric cancer. J Minim Access Surg. 2022;18:578-584.ArticlePubMedPMC
- 7. Zhu G, Lang X, Zhou S, Li B, Sun Q, Yu L, et al. Short- and long-term outcomes of single-port versus multiport laparoscopic radical gastrectomy for gastric cancer: a meta-analysis of propensity score-matched studies and randomized controlled trials. BMC Surg. 2023;23:223.ArticlePubMedPMCPDF
REFERENCES
Figure & Data
References
Citations
Citations to this article as recorded by 

Techniques in Jejunojejunostomy, Gastrojejunostomy, and Esophagojejunostomy in Reduced-Port Gastrectomy
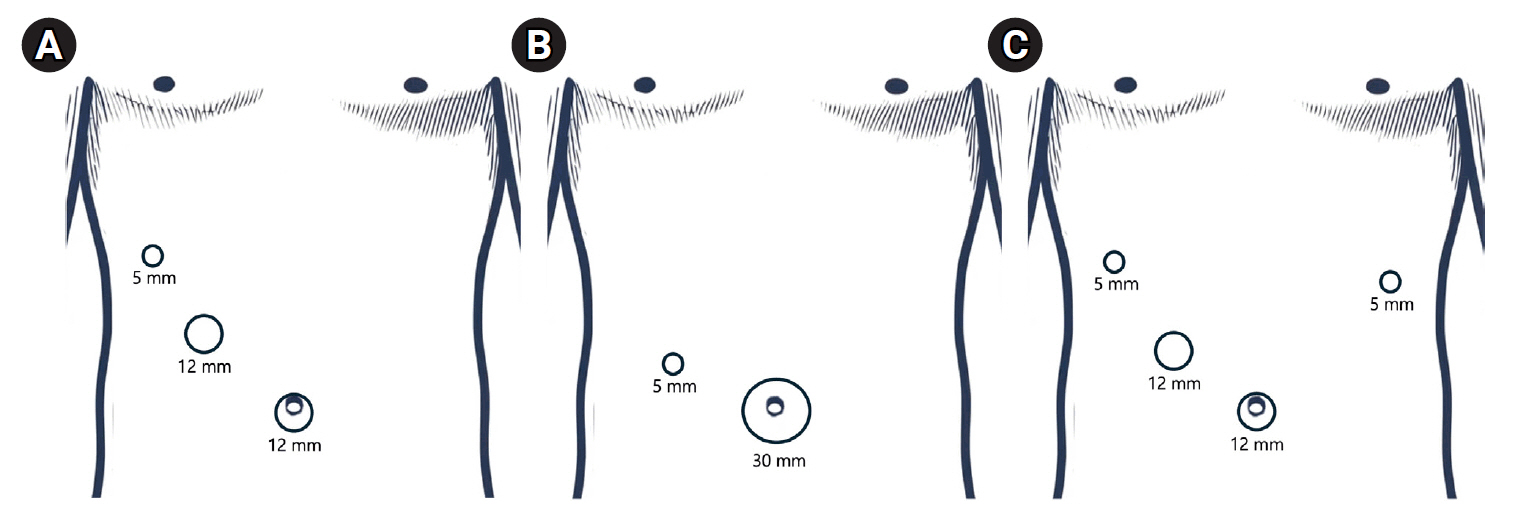
Figure 1. Laparoscopic port placements for the three cases. (A) Three-port surgery, (B) 2-port surgery, (C) 4-port surgery.
Figure 1.
Techniques in Jejunojejunostomy, Gastrojejunostomy, and Esophagojejunostomy in Reduced-Port Gastrectomy
TOP
 KSSSG
KSSSG
 PubReader
PubReader Cite this Article
Cite this Article